Articles / How sure do you need to be to treat for anaphylaxis?


writer
Paediatric Immunologist and Allergist; Staff Specialist, Sydney Children’s Hospital
Paediatric immunologist and allergist Brynn Wainstein says GPs often worry that they might not be making an accurate diagnosis of anaphylaxis, and wonder if they should still treat accordingly, even if the symptoms might actually be attributed to asthma an intercurrent illness.
His answer is a resounding yes.
“Remember that anaphylaxis is a medical emergency,” he says. “It’s an acute presentation, it can definitely be progressive and life threatening. And so it is important if you suspect anaphylaxis is occurring, to manage the patient appropriately. There really are no contraindications to administering intramuscular adrenaline, certainly in anaphylaxis, but also in most people. Intramuscular adrenaline is a really safe medication.”
“If you suspect anaphylaxis, even if you’re not 100% confident of what’s going on, treat for anaphylaxis. Give the intramuscular adrenaline.”
In fact, he tells parents whose children have asthma that if they’re unsure whether their child is experiencing asthma or anaphylaxis, giving them the auto injector will help either way.
“Adrenaline is actually really good treatment for asthma, it just doesn’t last as long as salbutamol.”
He says if you’re concerned about predicting risk in a patient with an allergy diagnosis, speaking to an allergist can help, but when in doubt his advice is the same: prescribe an auto injector.
How common is anaphylaxis to currently recommended vaccinations?
Overall, anaphylaxis to vaccinations is very uncommon, accounting for about one or two percent of all presentations of anaphylaxis,—and the trigger is usually an additive or an excipient in the vaccination itself, rather than the antigen in the vaccine, he says.
“So in a person who truly has allergy or anaphylaxis to an excipient in a vaccine, there may be a risk with other vaccines that have similar excipients, but it can be very tricky to diagnose,” he says.
Some people with latex allergy can appear to develop anaphylaxis to the vaccine–but what’s actually happening is they’re developing anaphylaxis to the latex and the stopper that is being collected in the needle as it’s pushed into the vial. But he says this is less of a problem now that multi dose vials have become less popular.
How can people find out if they’re likely to experience an anaphylactic or allergic reaction to a vaccination?
Ideally the way to do this is to sit down with a list of the excipients and the symptoms that have occurred— and try and decide what is most likely to have caused the reaction. Then in some cases you can do skin or intradermal testing with the excipient itself, or even a challenge with the excipient itself, to try to make the diagnosis.
“But sometimes it can be very tricky and in some cases, especially in children, the end result of all of this is to give the vaccine under supervision, understanding that even in a person with a history of an allergic reaction that was thought to be due to a vaccine (as opposed to an adverse event of a vaccine or an idiosyncratic reaction or something of that nature), sometimes the most logical way to handle the situation is to administer the vaccine in a suitable environment with suitably qualified trained personnel on site,” he says.
“There is always a risk of reactions or anaphylaxis, even in a person with no history. But the nice thing about vaccines is that once they’re in, they’ve been given. Sometimes just doing the test allows you to administer the vaccine and then the patient has the benefit of the vaccine, and perhaps a diagnosis of tolerance or otherwise. “
Is there a clear winner between adrenaline auto injector and the adrenaline in doctors’ bags?
Not necessarily, but it depends on the circumstances and who is administering it, he says.
Adrenaline auto injectors have a fixed dose of adrenaline in them, and so we make adjustments for that in the prescribing recommendations. But obviously, ideally, it is best to base the dose of adrenaline on the patient’s weight in terms of a 10 microgram per kilogram dose, wherever possible.
Now, auto injectors are designed for people with no medical training to be able to safely administer adrenaline in doses that are likely to work, even if they’re not necessarily ideal.
“The reason that we don’t recommend vials of adrenaline and needles and syringes to non-medically trained people or to parents –and I might add, even if those parents are doctors— is because of the risk of an error, especially in the heat of the moment where you’re trying to draw up adrenaline, and you’ve got a 1ml syringe and you’re drawing up very small volumes of a one in a thousand concentration…In that setting, it is definitely better to have an auto injector.”
“But if you have experience in administering adrenaline, in drawing up doses from vials, and you understand and know the dose and you have access to the appropriate equipment, then it is perfectly appropriate to use a needle syringe and adrenaline vial, provided that you are drawing it up correctly and you’re checking the dose before it’s administered. And it’s always useful, of course to get somebody else to check it as well. All of those things are probably more important than which device is better.”
There will be a demonstration of Epipen and Anapen at The Annual Women’s & Children’s Health Update in Adelaide, Brisbane, Melbourne, Sydney and Perth. Register now to an event near you and hear many more important topics affecting women and children.
For a verbatim version, watch Dr Wainstein answer GPs questions below.
Based on this educational activity, complete these learning modules to gain additional CPD.

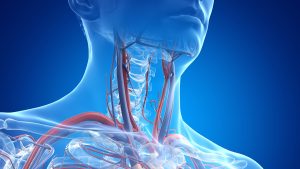
TIAs and Carotid Stenosis

HSDD - What is it & How is it Managed?

Functional Gastrointestinal Disorders in Infants (FGIDs) – Practical Advice for GPs

Using the New RSV Vaccine in Practice

writer
Paediatric Immunologist and Allergist; Staff Specialist, Sydney Children’s Hospital


Strongly support
Somewhat support
Neither support nor oppose
Somewhat oppose
Strongly oppose
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
You have completed the Educational Activities component of this resource.
Select ‘Confirm & claim CPD‘ to confirm you have engaged with this resource in its entirety and claim your CPD.
You will be taken to explore further CPD learning available to you.