Articles / Half of Australians in aged care have depression. Psychological therapy could help


writer
Professor of Clinical Psychology, Swinburne University of Technology
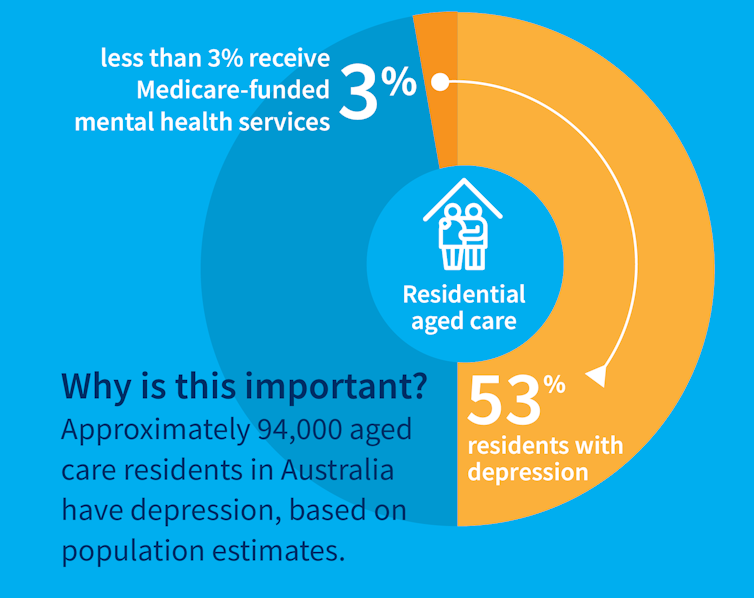
While many people maintain positive emotional wellbeing as they age, around half of older Australians living in residential aged care have significant levels of depression. Symptoms such as low mood, lack of interest or pleasure in life and difficulty sleeping are common.
Rates of depression in aged care appear to be increasing, and without adequate treatment, symptoms can be enduring and significantly impair older adults’ quality of life.
But only a minority of aged care residents with depression receive services specific to the condition. Less than 3% of Australian aged care residents access Medicare-subsidised mental health services, such as consultations with a psychologist or psychiatrist, each year.
Instead, residents are typically prescribed a medication by their GP to manage their mental health, which they often take for several months or years. A recent study found six in ten Australian aged care residents take antidepressants.
While antidepressant medications may help many people, we lack robust evidence on whether they work for aged care residents with depression. Researchers have described “serious limitations of the current standard of care” in reference to the widespread use of antidepressants to treat frail older people with depression.
Given this, we wanted to find out whether psychological therapies can help manage depression in this group. These treatments address factors contributing to people’s distress and provide them with skills to manage their symptoms and improve their day-to-day lives. But to date researchers, care providers and policy makers haven’t had clear information about their effectiveness for treating depression among older people in residential aged care.
The good news is the evidence we published today suggests psychological therapies may be an effective approach for people living in aged care.
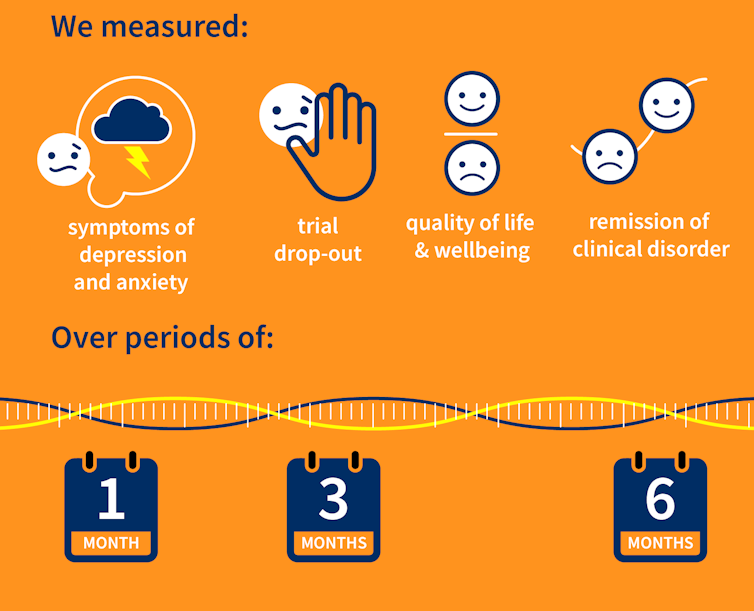
Our research team searched for randomised controlled trials published over the past 40 years that were designed to test the effectiveness of psychological therapies for depression among aged care residents 65 and over. We identified 19 trials from seven countries, including Australia, involving a total of 873 aged care residents with significant symptoms of depression.
The studies tested several different kinds of psychological therapies, which we classified as cognitive behavioural therapy (CBT), behaviour therapy or reminiscence therapy.
CBT involves teaching practical skills to help people re-frame negative thoughts and beliefs, while behaviour therapy aims to modify behaviour patterns by encouraging people with depression to engage in pleasurable and rewarding activities. Reminiscence therapy supports older people to reflect on positive or shared memories, and helps them find meaning in their life history.
The therapies were delivered by a range of professionals, including psychologists, social workers, occupational therapists and trainee therapists.
In these studies, psychological therapies were compared to a control group where the older people did not receive psychological therapy. In most studies, this was “usual care” – the care typically provided to aged care residents, which may include access to antidepressants, scheduled activities and help with day-to-day tasks.
In some studies psychological therapy was compared to a situation where the older people received extra social contact, such as visits from a volunteer or joining in a discussion group.
Our results showed psychological therapies may be effective in reducing symptoms of depression for older people in residential aged care, compared with usual care, with effects lasting up to six months. While we didn’t see the same effect beyond six months, only two of the studies in our review followed people for this length of time, so the data was limited.
Our findings suggest these therapies may also improve quality of life and psychological wellbeing.
Psychological therapies mostly included between two and ten sessions, so the interventions were relatively brief. This is positive in terms of the potential feasibility of delivering psychological therapies at scale. The three different therapy types all appeared to be effective, compared to usual care.
However, we found psychological therapy may not be more effective than extra social contact in reducing symptoms of depression. Older people commonly feel bored, lonely and socially isolated in aged care. The activities on offer are often inadequate to meet their needs for stimulation and interest. So identifying ways to increase meaningful engagement day-to-day could improve the mental health and wellbeing of older people in aged care.
Many of the studies we found were of relatively poor quality, because of small sample sizes and potential risk of bias, for example. So we need more high-quality research to increase our confidence in the findings.
Many of the studies we reviewed were also old, and important gaps remain. For example, we are yet to understand the effectiveness of psychological therapies for people from diverse cultural or linguistic backgrounds.
Separately, we need better research to evaluate the effectiveness of antidepressants among aged care residents.
Depression should not be considered a “normal” experience at this (or any other) stage of life, and those experiencing symptoms should have equal access to a range of effective treatments. The royal commission into aged care highlighted that Australians living in aged care don’t receive enough mental health support and called for this issue to be addressed.
While there have been some efforts to provide psychological services in residential aged care, the unmet need remains very high, and much more must be done.
The focus now needs to shift to how to implement psychological therapies in aged care, by increasing the competencies of the aged care workforce, training the next generation of psychologists to work in this setting, and funding these programs in a cost-effective way. ![]()
Tanya Davison, Adjunct professor, Health & Ageing Research Group, Swinburne University of Technology and Sunil Bhar, Professor of Clinical Psychology, Swinburne University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.
![]()

MHT For Women With History or Risk of Cancer

Muscle Health in the Elderly

GLP-1s For OSA

Oral Corticosteroid Stewardship For Asthma – Why it is Important

writer
Professor of Clinical Psychology, Swinburne University of Technology



Strongly agree
Somewhat agree
Neutral
Somewhat disagree
strongly disagree
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
Menopause and MHT
Multiple sclerosis vs antibody disease
Using SGLT2 to reduce cardiovascular death in T2D
Peripheral arterial disease
