Articles / GP mass exodus looming

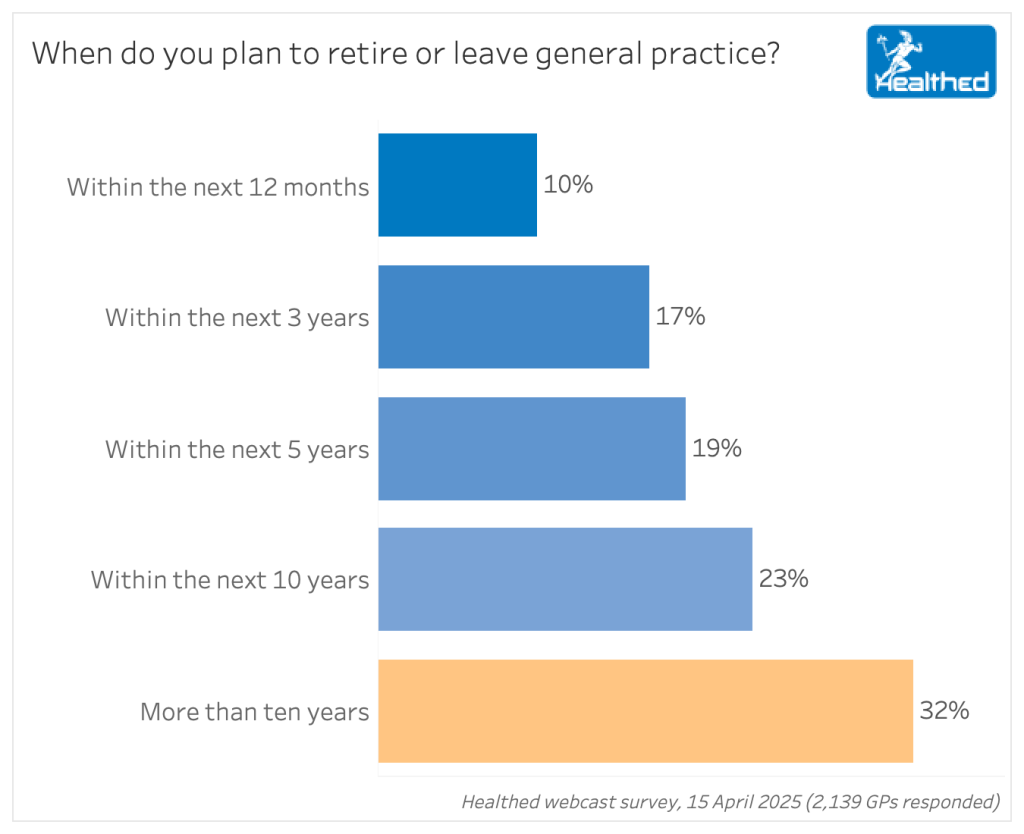
Primary care is teetering on a precipice, with 46% of GPs planning to retire or leave practice in the next five years, according to a national Healthed survey of more than 2000 GPs.
Not only will this bring a huge loss of experience, it could also tip our health system into crisis, experts say—and current polices are not enough to stem the brain drain.
We asked GPs planning to retire what’s prompting their decision. Unsurprisingly, age was by far the most common response, cited by 50% (521 of 1038 responses). The average age of GPs across Australia is 50.6, and more than one in seven GPs (15.7%) is 65 or older.
But more than half of GPs cited other reasons for leaving, including work stress, burn out, unnecessary paperwork, bureaucracy, lack of work-life balance and a feeling that GP work is not valued or respected.
“Though I love my job as a GP, the duress of red tape is a major hindrance to quality of patient care,” one doctor wrote, while another described themselves as “buckling under the burden of administration requirements.”
A GP in their early 40s said if it weren’t for global politics, they’d be exiting the profession early too.
“Thank Trump – I’m still working because my super balance has been affected. If I won Lotto, I would leave immediately. The admin burden, bureaucratic demands, AHPRA oversight is withering and killing my love of GP. For 10 minutes of patient care – more than half is now admin/paperwork/bureaucracy related.”
Experts say healthcare bureaucracy is largely to blame for the impending exodus.
“Government policy is so out of step with the reality on the ground,” says Clinical Associate Professor Aniello Iannuzzi, practice owner and chair of the Australian Doctors Federation.
“This is both sides of politics. There’s been 40 years of neglect since Medicare has come in. And every time there’s some problem in the health system, general practitioners get burdened with more and more blame, lack of respect, red tape. And quite frankly, general practitioners are getting sick of it, and they’re looking for alternatives.”
Dr Mukesh Haikerwal, former AMA President, who recently retired after 35 years in general practice, agrees, noting health policy is increasingly driven by bureaucrats, with less and less input from practitioners.
Decades ago, when the Health Insurance Commission ran Medicare, they consulted regularly with peak GP bodies; this no longer happens, but GPs are still bound by decisions made without their involvement.
“Cinicians overall – doctors in particular, and GPs acutely – are totally dealt out of the equation in decision-making and governance of the healthcare system, yet they’re the whipping boy for policy,” Dr Haikerwal says.
Associate Professor Iannuzzi says excessive red tape and poor remuneration indicate an underlying lack of respect.
“I’ve even heard of practice owners going to do shifts at urgent care clinics because they’ve worked out they’re better off doing that than working in their own practice.”
“And the fact that now overseas trained doctors can come in, get registered by AHPRA and just bypass the colleges, that’s further undermining confidence,” he adds.
If this trajectory continues, our health system is likely to unravel as more and more people turn to emergency departments, urgent care clinics, and telehealth services—none of which promote continuity of care, Associate Professor Iannuzzi says.
Dr Haikerwal says losing 46% of GPs would be a “calamity”.
“People who are of retirement age, you actually want to retain them until you’ve got the new lot trained up and ready to go,” he says.
“We want new people who have the courage and wherewithal to do things in general practice, rather than necessarily refer everything out. And that means that the people who have been there a while and got a bit more rubber on the wheels can actually continue in a way they want to help the new people coming through and have a peaceful transition,” Dr Haikerwal says.
Professor Karen Price, GP, researcher and past president of the RACGP, agrees we’ll suffer from the loss of experienced GPs who can mentor less experienced practitioners, along with the many “wise heads who’ve been around the block a few times” who can help colleagues facing “crises of faith or of practice.”
We also risk losing much “deep relational expertise” that helps stop patients “jumping around to 10 different practitioners and using unproven treatments and spending their precious healthcare dollars on nonsense,” she says.
The brain drain could also adversely affect population outcomes, she adds.
The Government has committed to an extra 2000 trainee positions each year, and IMGs from some countries can be fast-tracked into practice.
But it’s not enough to fill the gaping hole that will be left as the most experienced GPs leave, experts say.
Professor Price notes the recent election did not deliver any real reform.
“There’s signs of resuscitation—a thready pulse—but they haven’t fixed the fundamentals,” she says.
“They, in fact, embedded some of the challenges of the system with high volume, fast throughput, and projected that as a solution, which we all know it’s not,” Professor Price says.
“And we still have not addressed mental health, aged care, chronic complex health conditions and the demands they place on GPs.”
The system needs fundamental reform to make GP attractive, Professor Price says.
“These are highly qualified people who’ve got a range of choices at the beginning or middle or even end of their careers. They can go on and do other things. So we need to look after their workplace for them.”
This will require creative approaches and some flexible thinking from policymakers, rather than linear thinking and top-down operational models, she says
Associate Professor Iannuzzi agrees the system needs a complete reboot.
Rebates must be raised to make GP viable, Associate Professor Iannuzzi stresses.
“There’s a bulk billing incentive, there’s PIP—but until they do something serious about the rebates, we’re going to keep going down the gurgler.”
Dr Haikerwal agrees bulk billing incentives are not enough, emphasising that we need to support chronic disease management and longer consults, and “have an arm’s-length independent authority that sets the Medicare rebate based on the true cost of running a service.”
“By all means, put $8.3 billion in, but when your bulk billing incentive scheme doesn’t work, and your plan to nationalise general practice by stealth and on the cheap fails, then keep the $8.3 billion and let’s spend it in a better way.”
To do that, policymakers need meaningful engagement with the peak bodies, he says. Not just election promises, but really listening, responding, and implementing.
Regulation has become increasingly onerous and the accreditation process—which started with good intentions—has “run amok,” Dr Haikerwal says.
Associate Professor Iannuzzi agrees accreditation has become increasingly stressful and irrelevant.
“They’ve just gone nuts with their proliferation of standards. And practices are only doing accreditation to get access to the blended payments. It’s got nothing to do anymore with genuine striving for excellence.”
“The College of GPs has to actually start doing what they’ve been promising for a while. And that’s make the standards much simpler, and much more focused on what actually is relevant to patient care,” Associate Professor Iannuzzi says.
Professor Price can understand some increases in regulatory oversight and documentation, but “the scope creep of that has been pernicious upon the workforce,” she says.
And digital solutions are not a pat answer. “The so-called digital revolution has helped the tech bros, but it’s yet to be determined how well it’s supported workflows,” she says, noting interoperability remains a major problem, and individual workarounds often add to the documentation burden.
“So there are probably a million different ways that that could be streamlined.”
Associate Professor Iannuzzi would like to put general practitioners back into big teaching hospitals.
“That way we have visibility, it will address the respect issue, it will address the recruitment/retention issue.
“Junior doctors can actually see that we’re not dumb; that we can make meaningful improvements.”
Professor Price cautions against the over-commercialisation of medicine.
“What I’m concerned about is that everything’s now got a dollar attached to it,” she says.
“Some economists talk about the medical market, but we’re a profession and I think that needs to be remembered both by politicians, patients and by practitioners.”
“We really do need to begin the reform or we’re going to find that we have a merchant-based system. And I don’t think that will serve us or patients very well.”

Autism Spectrum Disorder – Managing Challenging Behaviours

Paediatric Allergic Rhinitis & Immunotherapy

Premature Ovarian Insufficiency – The New Guidelines

Alcohol Addiction Assessment and Advice


Increase
No change
Decrease
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
