Articles / Medicare changes – We’ve been sold a pup!
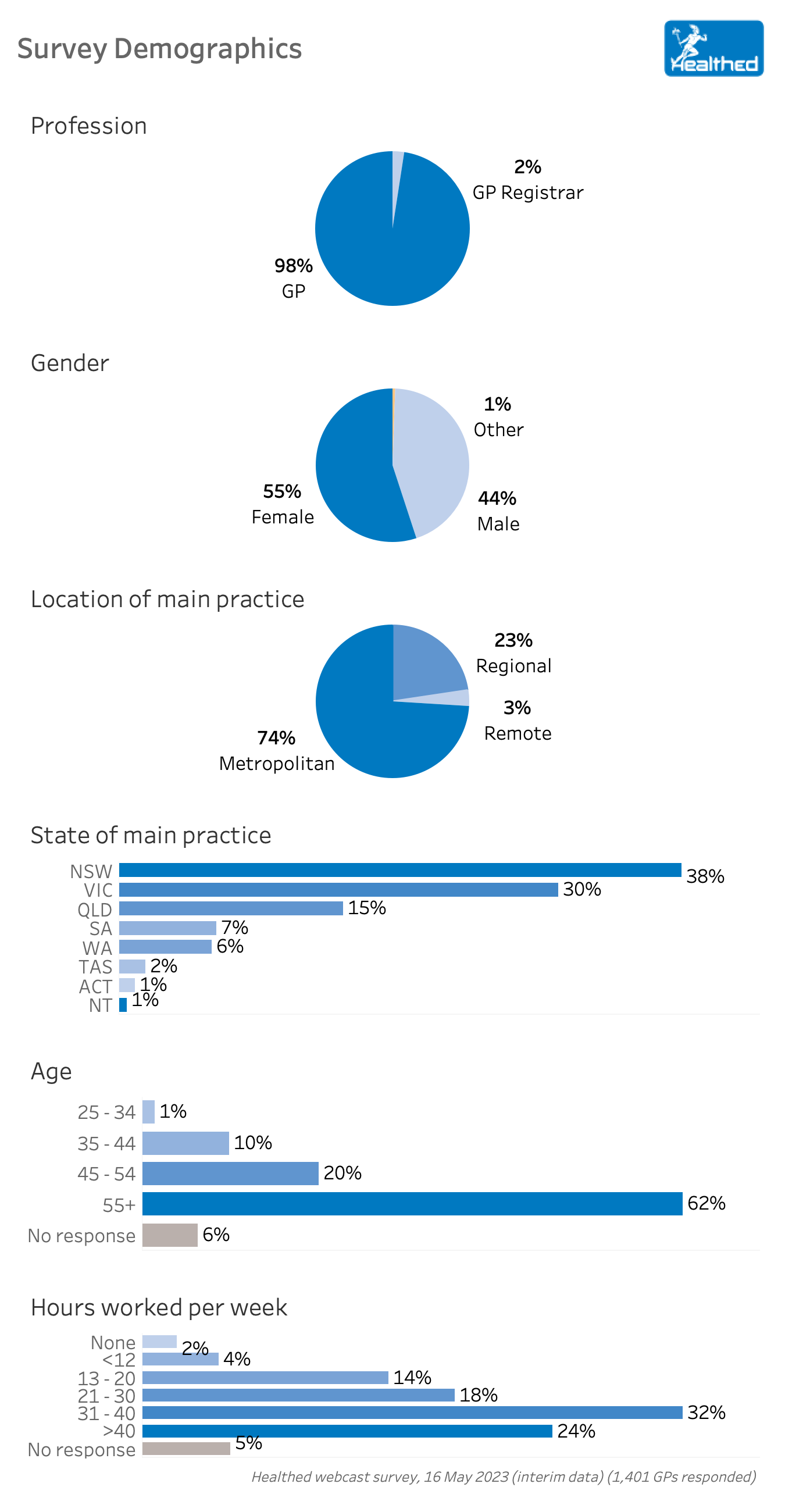
Despite much praise from the RACGP and the AMA, Healthed survey data from 1200 GPs across Australia suggests that the recently announced Medicare changes will do little to reverse the erosion of Medicare.
‘We’ve been sold a pup,’ summed up GP and past president of the AMA, Dr Mukesh Haikerwal, who now also helps lead the Australian GP Alliance, and has been vocal in his concerns that the changes don’t go far enough.
The vast majority of surveyed GPs said the budget measures would have no impact on the gap fee they charge or the number of patients they bulk-bill — though 15% of respondents said the size of the gap fee they charge will likely increase, and 15% expected the number of patients they bulk-bill to go down.

Dr Haikerwal hypothesises that these GPs were already planning to increase the gap fee to cover rising costs, and the bulk-billing incentives aren’t enough to off-set this. He also reckons it’s wishful thinking to assume the incentive will give some enough of a leg up to reduce their costs: “when push comes to shove that won’t happen but that’s their hope, I guess…”
“For 15 years there’s been no increase in rebate indexing, it’s been 0.5% a year for the last 10 years. Nothing else has stayed at that level, everything has grown in cost and expenditure,” he says.
“The changes are in the right direction, but nowhere near enough to make up for the nine years of Medicare freeze and current inflation for practices to pay their bills, and that’s why we’ve been forced to change to mixed billing,” one surveyed GP lamented.
While most GPs feel the changes outlined in the budget are trending in the right direction, the overwhelming sentiment is that they don’t go far enough to create real change.
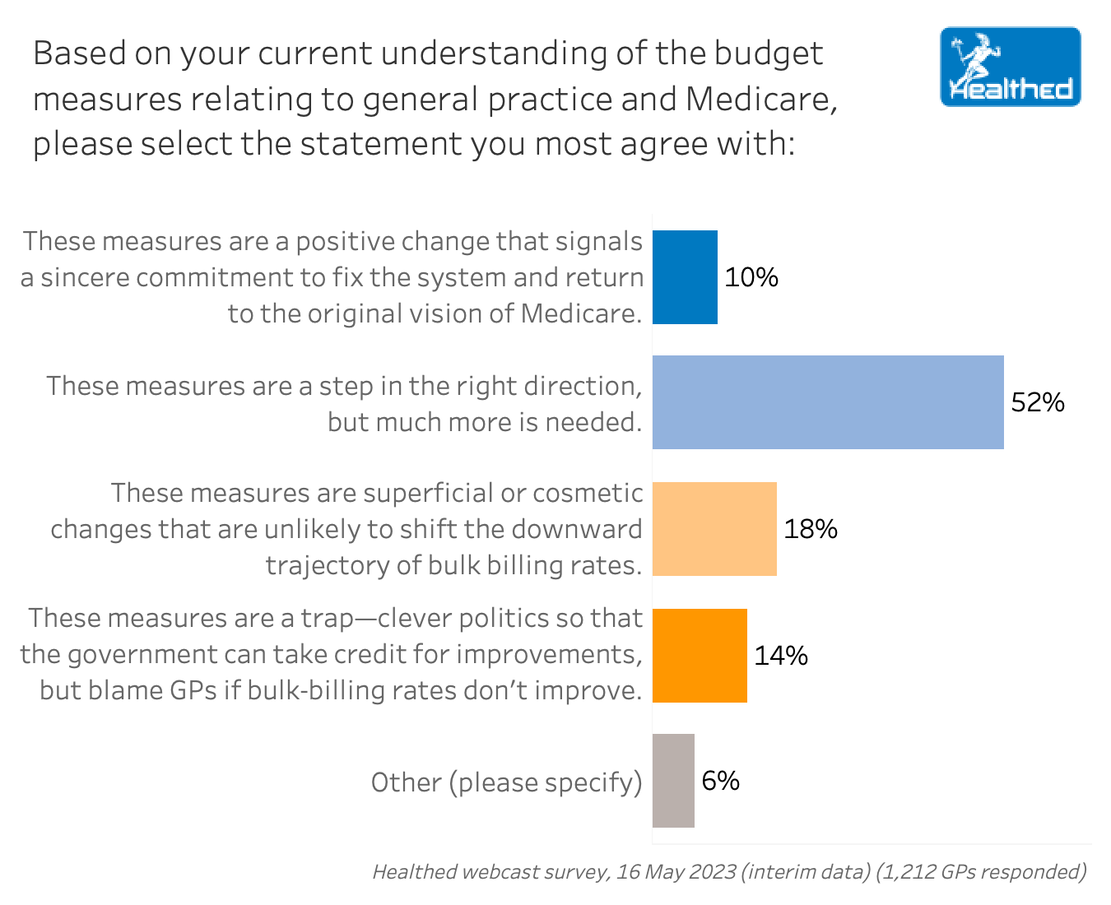
Clinical Associate Professor Pradeep Jayasuriya is among those arguing that the Medicare changes are a trap which move us closer to a two-tiered system. “If it’s successful, the government can take credit, and if it fails, GPs can be blamed,” he wrote in an op-ed for Healthed.
Dr Haikerwal agrees. He says the policy allows the government to claim they’ve given the money, knowing all the while that it won’t be enough, and allowing them to defray the cost arguments to ‘the greedy doctor’.
“The goodwill of doctors is being exploited,” Dr Haikerwal says, harkening back to a Press Club speech he gave circa 2005, and adding that nothing’s changed in all those years.
While some who already bulk-bill may indeed be better off financially once the changes come into effect, Dr Haikerwal also points out that the budget notes upcoming “efficiencies” (AKA cuts) to chronic disease management planning MBS item numbers that have yet to be fleshed out.
“We don’t know what the other clawbacks are going to do,” he says. “That’s the big problem.”
Dr Haikerwal highlights some small budget wins—such as the plan to establish a Centre for Disease Control which will hopefully reduce the chances of another disconnected response like we saw in COVID, and increased funding for nurses and psychology students.
However, he remains concerned that rejigging the MBS item numbers and a focus on compliance rather than fixing the overly complex system could further reduce access to care for the 50% of Australians with chronic diseases. “That clawback is potentially going to be a hazard on the biggest game in town, which is chronic disease management,” Dr Haikerwal said. “And if you then link it to voluntary patient enrollment, that is potentially a disaster if it’s handled badly.”
What your colleagues are saying
6-minute minimum ignores all the work that happens after the patient leaves…
“Setting a minimum 6 minutes for Level B consult completely disrespects and disadvantages experienced GPs who can manage complex issues in less than 6 minutes of patient contact time and ignores the fact that unpaid work coming out of a less than 6-minute consult (referral letters, chasing results etc) done in GPs own time in order to allow more patients to access appointments will make even less appointment slots available. Not well thought out. Level B should be based on complexity and under 20 minutes with no lower limit.”
Changes reward ‘churn and burn’ medicine
“I am disappointed that the changes essentially reward “churn and burn” medicine as the increased bulk billing rate benefits those doing a lot of short consultations more than someone doing a lot of longer higher quality consultations. I would like to see item numbers increase by 10-minute increments.”
Under-billing needs to stop
“Many of my patients are aged pensioners who I will most likely continue to bulk-bill. I have started to bulk-bill appropriate time spent by myself and our nurses on the patients with difficult complex wounds that can sometimes take up to an hour to dress not including costs of dressings, and other comorbidities, as I believe we have seriously under-billed Medicare for such patients in the past. It is our grassroots GP services that are keeping these patients out of the more costly hospital care and saving the public purse, so it is only appropriate that we bill for our time appropriately.”
GPs call BS on the ‘greedy doctor’ narrative
“There is little mention about the poor and unsustainable conditions that GPs are working under. We have taken a decrease in pay, have greater professional requirements and are the ‘whipping post’ for the government – there is little, if any, recognition of the reasons that GPs had to stop bulk-billing. They portray it as if we are greedy and trying to make more money – no mention that we are no longer able to keep our doors open and cannot find GPs in regional areas because it’s become such an undesirable job!”
It’s a trap
“Political smoke and mirrors! Medicare rebate frozen for years. Bulk billing INCENTIVE x 3 but NOT service fee… Patients will not understand the change and think GPs are greedy.”
Catch 22 for GPs
“I don’t think the ‘millions’ invested in general practice actually equates to increased renumeration to GPs. If there is no change to the Medicare rebate for the common items for GPs to claim from, we will continue to charge more based on indexation and inflation. The end result is the patient suffers as a larger gap will be created. Nurses and GPs work more than they are being paid for. We suffer the indignation of being unable to charge what is really necessary because we feel our patients’ care will suffer if we charge the full rate.”
Concession card holders should be bulk-billed
“I agree that the Medicare rebates are very low. However, several GP practices have gone a bit too greedy when they do not bulk-bill concession card holders. They need our services the most, are disadvantaged and have no reserves financially to absorb the increased cost of living. Some GPs have lost their sense of humanity unfortunately.”
UK model not one to follow…
“Capitation does not work. I escaped the UK NHS model 35 years ago for this exact reason. You have the most intelligent, qualified people within society being paid $24 an hour as reward for getting up at 3 a.m. to assist in a child’s delivery.”
You can’t make patient care a numbers game
“Patient registration and using it for control of payments to GPs would be a disaster for patients and encourage cherry picking by those who are more interested in systems and control than genuine patient care. You cannot make patient care and outcome a numbers game…Further disincentive for GP recruitment.”
Gee thanks…
“We are supposed to be thankful after 10 years of less than 50-cent increases for Level B consultations. The ageing population means longer consults and charging a Level B to stay under the radar is probably commonplace. A Level B is less remuneration than the podiatrist /physio and we treat people to keep them out of hospital.”
Survey conception and design – Dr Ramesh Manocha, Yasmin Clarke, Lynnette Hoffman
Writing and reporting – Lynnette Hoffman
Survey analysis and visualisation – Yasmin Clarke

Heart Failure – Assessment and Monitoring in Primary Care

Heart Failure – Demystifying Pharmacological Management for GPs

COPD Update

Iron Deficiency in Children & Young People



Strongly support
Somewhat support
Neither support nor oppose
Somewhat oppose
Strongly oppose
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
You have completed the Educational Activities component of this resource.
Select ‘Confirm & claim CPD‘ to confirm you have engaged with this resource in its entirety and claim your CPD.
You will be taken to explore further CPD learning available to you.