Articles / AHPRA says vexatious complaints are very rare, GPs disagree

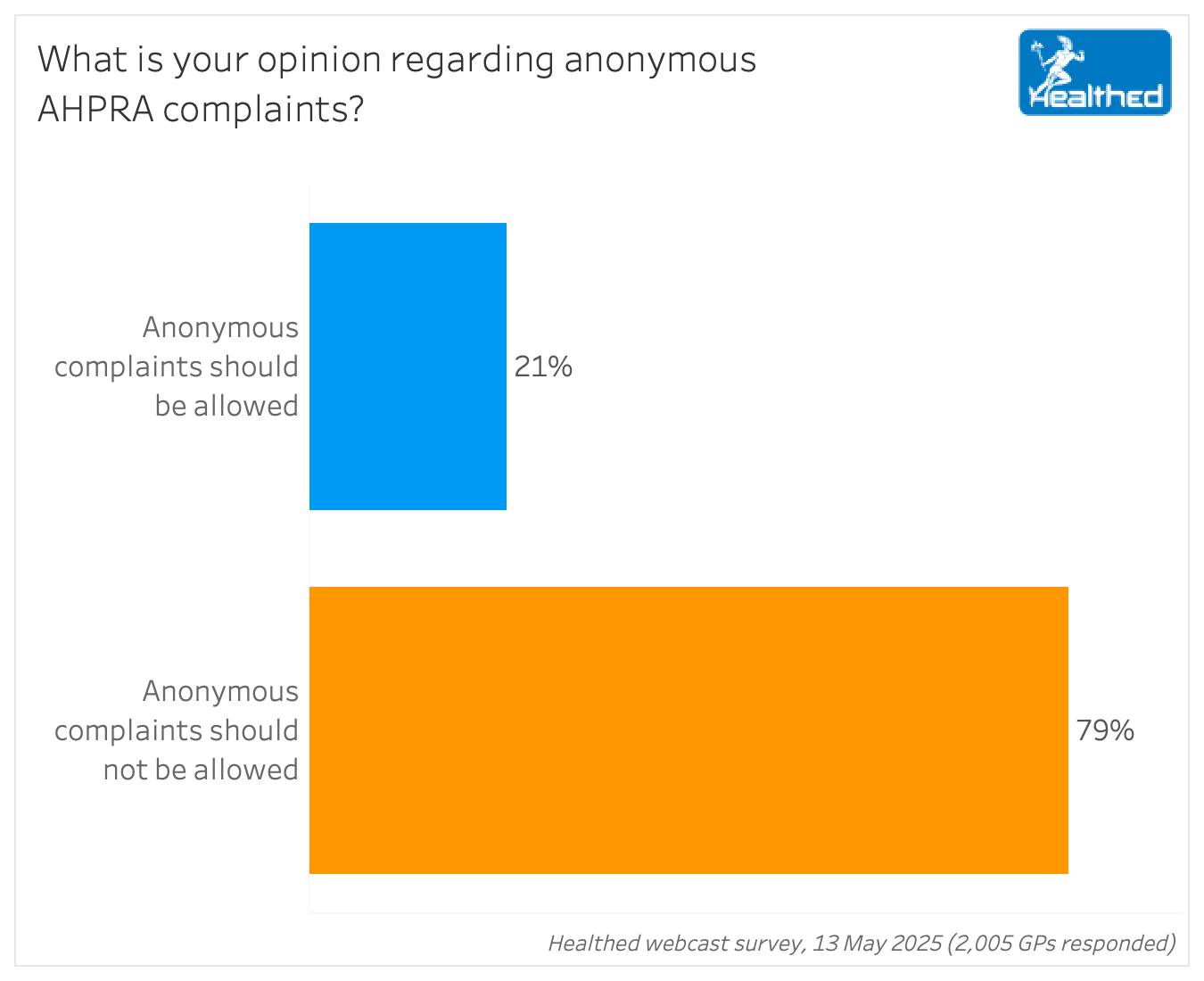
Eight out of 10 GPs say anonymous complaints to AHPRA should be banned, but with the policy unlikely to be overturned, how worried should we be?
A review published by the National Health Practitioner Ombudsman (NHPO) in December found that while the number of vexatious notifications made every year is likely to be low, “Ahpra has not appropriately recorded all instances where a practitioner alleged that a notification was made vexatiously,” noting that the framework for identifying and managing vexatious complaints should have been applied more frequently than it was.
“Ahpra should ensure allegations that a notification is vexatious are appropriately documented and managed in line with the Framework, with relevant information about the assessment of the allegations recorded and provided to decision makers for consideration,” the Ombudsman’s review recommended.
A spokesperson for AHPRA told Healthed that the agency received 120 notifications from anonymous notifiers between 1 July 2022 and 31 May 2025.
That equates to 0.6% of all notifications received about medical practitioners, they said, adding that during the same period, AHPRA completed 162 notifications where the notifier was anonymous.
Of those completed matters, AHPRA’s spokesperson said 144 (89%) resulted in no action.
“For one of the ‘no action’ matters, the board found that the matter was vexatious,” they said, adding that 18 of the anonymous complaints resulted in regulatory action or referral to tribunal regarding concerns such as practising while suspended, inappropriate sexual relationships, inappropriate prescribing of schedule 8 medications and alleged criminal conduct.
“For each of these notifications, the Board relied on information that supported the action gathered from either the practitioner’s records or submissions, or from third-party sources,” they said, noting that some notifications were received before the reporting period or were identified as anonymous later, for example because a pseudonym had been used.
Clinical Associate Professor Aniello Iannuzzi, practice owner and chair of the Australian Doctors Federation said AHPRA’s response was “somewhat dismissive.”
“As much as they want to make it sound like it’s negligible, the absolute number of doctors being subjected to a procedural lack of fairness is still significant,” Associate Professor Iannuzzi said.
He noted that along with anonymous notifications, complaints from organisations, or from people who aren’t even connected to the care, such as vexatious colleagues and staff members, can also be problematic.
The Ombudsman’s review also highlighted a disconnect between health professionals’ perceptions of the volume of vexatious notifications compared with “true instances” according to the available evidence. It said the conflicting views seemed to stem from differing definitions of ‘vexatious,’ with health professionals believing the complaints are disruptive and inconvenient, and don’t generally consider the notifier’s intent.
“The review found that sometimes the term ‘vexatious’ is used to describe any type of sub-optimal notification, including notifications that are lacking in substance.”
But AHPRA’s definition “focuses on the motivation of the person making the notification, rather than only the experience of the practitioner subjected to the notification.”
“While the motivational definition sets a high threshold for determining a notification is vexatious, the review contends that this is reasonable and aligns with the gravity of labelling a notification vexatious,” the Ombudsman report stated.
AHPRA has also pointed to a report it commissioned in 2017, saying “there is greater risk of people not reporting concerns than of people making truly vexatious complaints.”
However, the majority of GPs who commented in Healthed’s survey disagreed.
“Completely unfair with no opportunity to respond,” one doctor said of anonymous complaints. “The small advantage of encouraging real, anxious complainants can be met by alternative methods.”
Many GPs believed that a higher proportion of anonymous complaints are malicious, vindictive, frivolous or vexatious — with several noting that anonymity makes it harder to investigate or respond effectively.
“When anonymous, they minimise the chance of working out the real problem,” one GP commented.
“How can a complaint be validated or investigated if it is from an anonymous source? Confidential yes, anonymous no.” – Surveyed GP
“Anonymity allows for falsehoods, fabrications and exaggerations more than if they had to put their name on the complaint. AHPRA needs to investigate the person making the complaint as much as the professional,” another GP said, adding that doing so would help to identify those who repeatedly lodge complaints or those with a history of doctor shopping, for example.
The NHPO report called for more transparency and better public reporting on decisions to take no further action on notifications, as well as a lower threshold for considering a ‘suspected vexatious’ notification, among other recommendations.
AHPRA has published a response on its website, stating that “The review is now complete and has made recommendations which Ahpra is implementing.”
AHPRA did not, however, respond to repeated inquiries from Healthed over more than two weeks regarding what progress it has made on actioning those recommendations.
The review also noted an inconsistency in the National Law. “It appears to be an offence to provide false or misleading information to Ahpra if a notification is being investigated but not at other stages of the notifications process. The review therefore recommends that Health Ministers should consider amending the National Law to make it an offence to provide false or misleading information to Ahpra when making a notification and at the assessment stage of the notifications process.”
Again, AHPRA did not respond to requests for comment on this matter.
What your colleagues are saying
“Anonymous complaints need to be restricted and carefully assessed before acting.”
“A complainant shouldn’t be allowed to hide behind anonymity, because this creates an avenue for baseless complaints to be made whether out of animosity, jealousy or other unsubstantiated reasons.”
“Legal action against false claims should be considered.”
“Anonymous complaints should be allowed, but only when supported by reasonable justification. Without such justification, it opens the door for potentially unfounded or malicious complaints, which is not appropriate.”
“They should be looked at with more caution than if the author is known.”
“Anonymous complaints should be recorded, but only investigated if serious, or if a pattern of complaints exists for a practitioner.”
“Complainants should be accountable. Anonymous allows falsehoods to go unchecked.”
“Anonymous complaints should only be allowed if there is a good reason for the complainant to remain anonymous. As the process is extremely stressful for doctors, I feel it is too easy for vindictive persons to hide behind anonymous complaints.”
“There should be a lodgement fee, refundable if the claim is upheld.”
“Australian law presumes innocent until proven guilty and this does not follow our rule of law.”
“It is important that all complaints be assessed. Some patients may feel unable to complain for fear of any reprisals.”
“Anonymity allows spurious complaints without the practitioner being able to clarify what occurred.”
“When such complaints can trigger immediate regulatory action, the impact on a practitioner’s career and mental health can be devastating. Transparency, fairness, and the right to respond fully require the complainant to be known. Legitimate concerns can still be handled discreetly without sacrificing due process.”

Autism Spectrum Disorder – Managing Challenging Behaviours

Paediatric Allergic Rhinitis & Immunotherapy

Premature Ovarian Insufficiency – The New Guidelines

Alcohol Addiction Assessment and Advice


Increase
No change
Decrease
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
