Articles / Medical misogyny headline grab misses the real issues, GPs say

Earlier this year The Sydney Morning Herald and The Age published an 11-part series based on interviews with 1800 women who say they’ve experienced medical misogyny firsthand.
Their accounts included stories of misdiagnosis and delayed diagnosis, as well as concerns that their pain or symptoms were downplayed or ignored, and often a feeling that they weren’t believed—all of which they attributed to misogyny.
Yet while most GPs acknowledge the underlying disparities, many take issue with the framing.
Nearly seven out of 10 GPs (69%) believe the media are either overplaying the situation or understand it poorly, according to a national Healthed survey with over 2000 GP respondents.
“There is clear evidence that gender bias exists in healthcare, but while media coverage has helped highlight this issue, the complexity of medical misogyny is often oversimplified,” one GP wrote.
Professor Karen Price, a GP, researcher, and former RACGP president, says victim-centred, blaming-type conversations seen in the media and on social media are “not a constructive way to solve inherently structural issues.”
“When you call something misogynistic, you’re suggesting that doctors don’t care en masse, and as a female doctor who’s worked a lot in women’s health, I find it insulting,” Professor Price says.
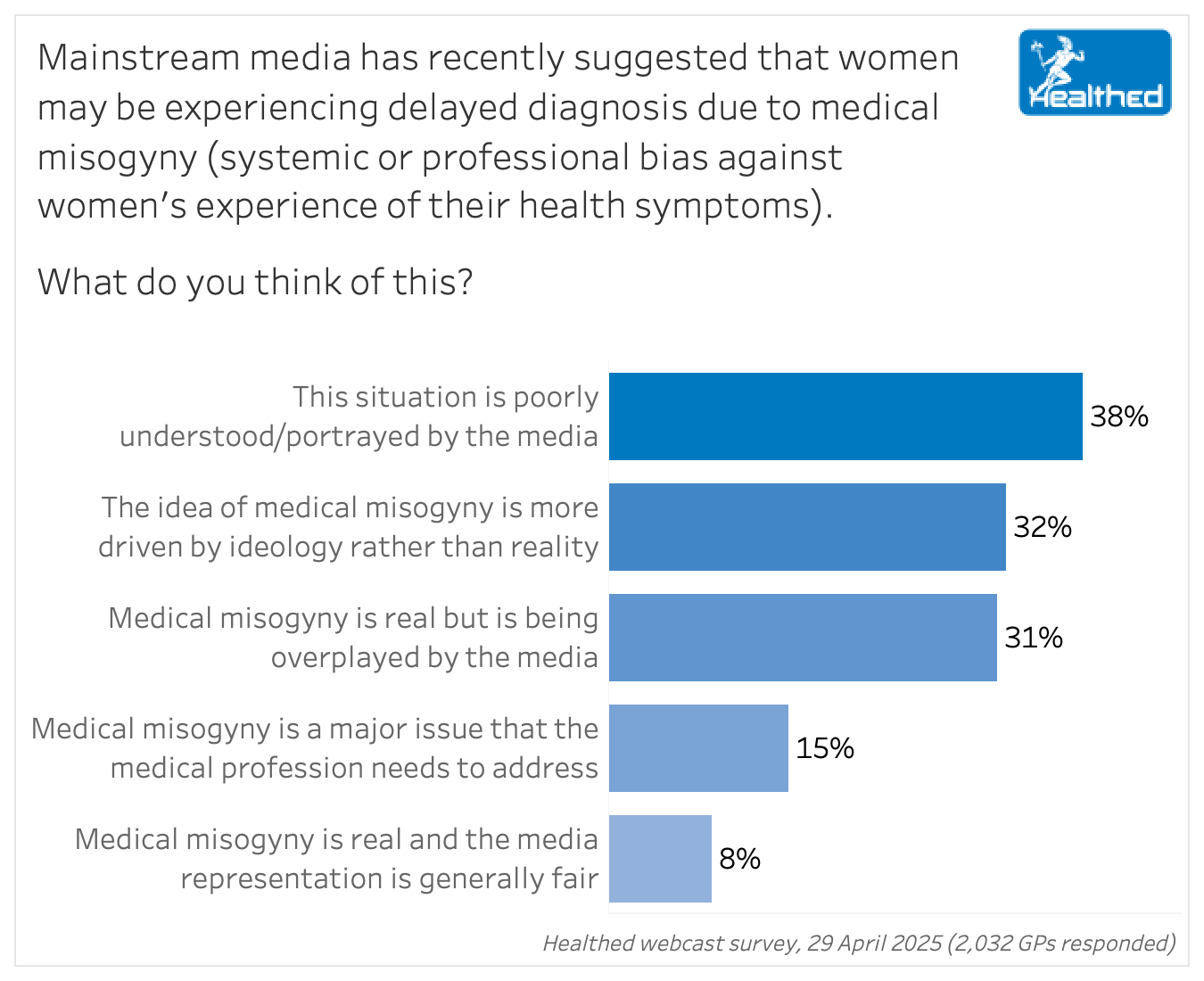
Overall, 54% of GP respondents were female and 46% were male. A similar proportion of males and females said the situation was poorly understood or portrayed by the media, while females were more likely than males to say that misogyny was real but being overplayed by the media. Males were more likely than females to attribute medical misogyny to ideology rather than reality.
Research does show discrepancies in care and health outcomes between men and women. A literature review commissioned by the Australian Government found women disproportionately experience delayed diagnosis, polypharmacy, and lack of investigation into their symptoms, and are less likely to get appropriate care than men.
Women’s needs are also underrepresented in clinical guidelines, and the National Women’s Health Strategy notes women are at higher risk of mental health disorders, dementia, and coexisting mental and physical illness. The gender gap for conditions such as heart disease and obstructive sleep apnoea is also well documented.
“To call it medical misogyny really harms the very people who are actually trying to work in this space, and it’s a very superficial thing, so let’s talk more constructively about it,” Professor Price says.
Managing complex issues like endometriosis and multi-morbidity takes time and continuity of care, and the system is not set up to support that.
Medicare reform is crucial to addressing that, she says.
“Medicare has inherent bias towards short consultations and everything the government has done has now rewarded high volume care,” Professor Price says.
“To get someone back three times because you’re bulk billing and only able to see one problem has a productivity penalty, so it’s not an efficient way to run a health system with complex needs.”
Meanwhile, patients are increasingly quick to change doctors if they don’t get what they want, making it harder for GPs to go through the “ruling in and ruling out” diagnostic process often needed to address women’s health concerns, Professor Price says.
“Complex care will need a complex solution, so that means we need longer consults. Doctors need time to care. They need time to work through those processes.”
Professor Price, and many doctors in Healthed’s survey, also point out that most GPs are working incredibly hard to support their patients with complex issues with empathy and thoroughness.
“Many, if not most, of us work extremely hard to actively listen to, and take absolutely seriously, symptoms and complaints of patients even when we suspect that the underlying problem is not likely to be anything sinister,” one GP commented.
“The extra time (and energy) taken is often not rewarded by Medicare so is at our own expense. That many of us ‘bust our gut’ to try to ensure that all symptoms or distresses are taken seriously and actively listened to, must be included in any discussion of ‘medical misogyny’.”
Professor Price adds that the research bias and medical education of yesteryear also play a role.
“I mean, I was taught that chest pain is a central crushing, left arm type of thing, and we now know that women present in very different ways,” she says, adding that even in laboratories researchers used male rats.
“It takes time to unpick those assumptions that were laid down 30 or 40 years ago, and to blame current generations for that is a bit unfair,” she says. Blaming just stops people from fixing the problem and working together to iron out some of those issues.”
Professor Price says ‘medical misogyny’ was coined during the heat of an election, potentially to draw attention away from underlying issues.
“A lot of mischief is made with politicians trying to win elections and using populist memes and studying all the trends in social media and jumping on bandwagons of blame, which is a misdirect if we’re going to fix the system.”
Labelling the problem as medical misogyny constitutes a breach of trust for many doctors, she adds.
“By using those terms, the government has broken trust with a large proportion of the medical profession, and that means they’ve broken the social contract, healthcare delivery for patients.”
She’s keen to see a move away from the dialogue of blame.
“Maybe it does sell newspapers because we get a bit of conflicted outrage, but that’s all it is, and it’s distracting the population from the real issues and being able to actually make sensible decisions when they cast their votes for whichever party they believe is going to manage those issues.”
What your colleagues are saying…
“The term medical misogyny is somewhat of a misnomer, for what is in reality gender-based neglect, secondary to time constraints, poor communication and lack of understanding of gender specific medical issues.”
“I absolutely see many women whose symptoms have been dismissed as ‘not too bad’ when they are having significant effects on their wellbeing and they feel so unheard and hurt by this.”
“I am very saddened that the good work/medical outcomes for women over many years are overridden by media backlash. Death rates for women in pregnancy have gone down. We are keeping babies alive that in the past would have died. No one accounts for this. Doctors keep more people alive than ever, compared with the past. There is an unfair expectation that everyone can be treated in a timely manner.”
“I believe medical misogyny is a decreasing problem in terms of deliberate bias. It is a problem in that there have been so many research studies excluding women, that we don’t have good data for women – especially in the area of cardiovascular disease for example.”
“Many of the so-called medical misogyny stories can equally affect males and females and do not result from a discrimination of the women. A patient with a headache or migraine can turn out to have a aneurysm- diagnostic errors can happen in both males and females.”
“I do think some male doctors have some regrettable opinions, and some have very little knowledge of how to manage simple female health issues, such as menopause. However, due to exaggerated claims by people on the internet, the problem is portrayed as much worse than it really is. Some N=1 accounts on the internet get excessively amplified, and suddenly it seems to be a systemic issue.”
“Lack of continuity of care and patient/GP relationships over time, and sausage machine bulk billing clinics, are a large part of the problem – as well as lack of funding for longer consultations.”
“I think a lot of both male and female doctors do not dive deeply into female physiology and psychology, doctors are really too focused on shorter consults and palm them off to someone else or leave them for later. Even some women feel that their symptoms are due to being on a particular time of their cycle or being perimenopausal.”
“Media that has to create issues to attract attention.”
“Sure there are woman haters in the medical profession, as in society at large. However, the examples I have read in the press recently are of delayed diagnoses due to the complexity of patient presentation, rather than malevolence. I’m sure men, if asked, could report delayed diagnoses too.”
“Medical misogyny is real but there is no discussion around the fact that some diagnoses are uncommon or difficult to diagnose and that these factors are important. Many women that are dismissed or misdiagnosed seek a second opinion from me and from their stories, I believe a lack of knowledge by the doctors has been a large contributor.”

Autism Spectrum Disorder – Managing Challenging Behaviours

Paediatric Allergic Rhinitis & Immunotherapy

Premature Ovarian Insufficiency – The New Guidelines

Alcohol Addiction Assessment and Advice


Increase
No change
Decrease
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
