Articles / Patients with eating disorders are seeking — and getting — GLP-1s

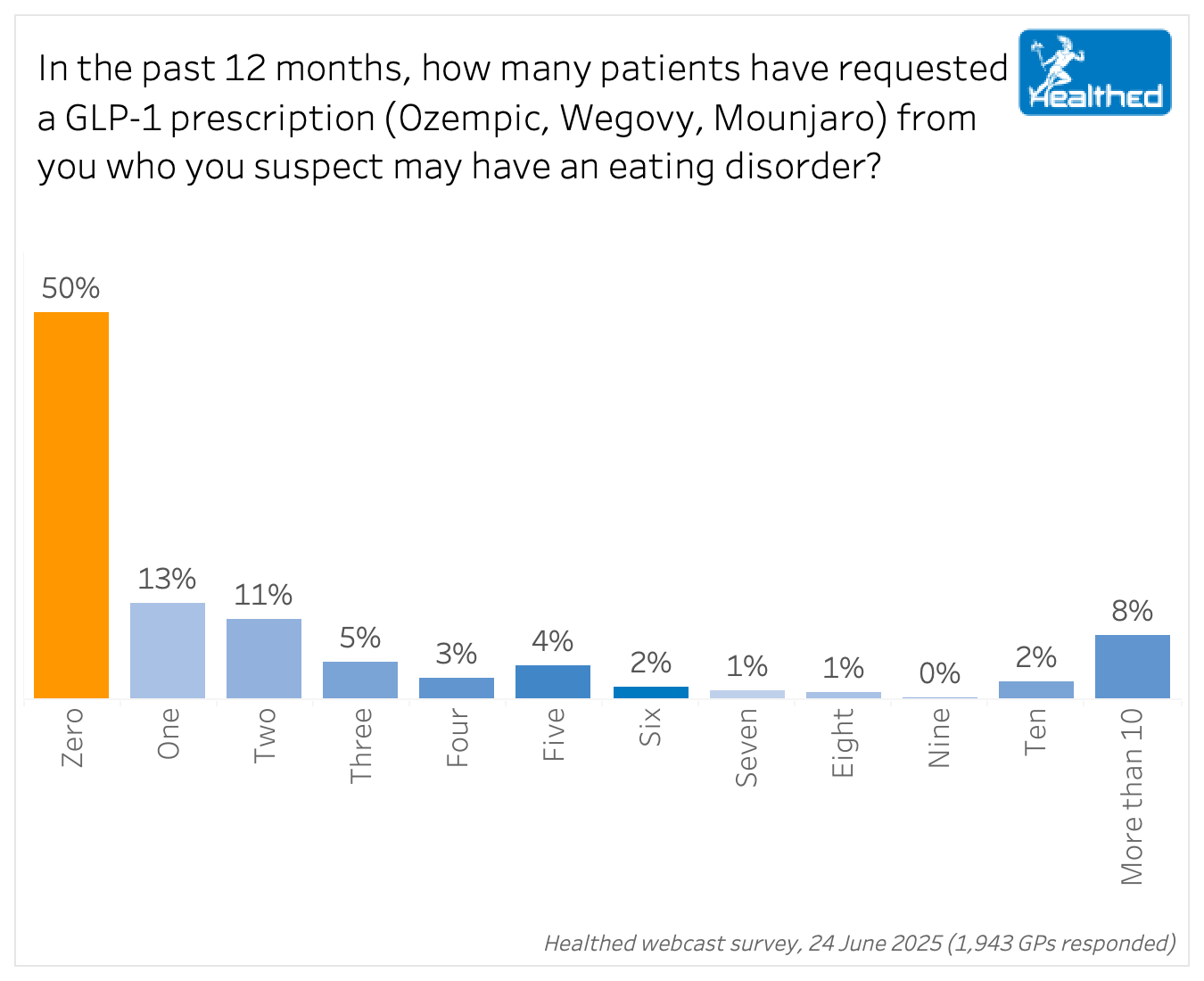
One in two GPs have had a patient with a suspected eating disorder ask for a GLP-1 script in the past 12 months, and one in four have encountered at least one patient with a suspected eating disorder who has successfully obtained an inappropriate prescription for a GLP-1, a Healthed survey of 1943 GPs has found.
Dr Jim Hungerford, CEO of the Butterfly Foundation, says weight-loss medications are marketed as a “quick fix”, making them “extremely attractive” to people with eating disorders, but they can have tragic consequences.
The drugs can worsen harmful thoughts and behaviours for people with an existing eating disorder—as well as contribute to an eating disorder developing in those who are vulnerable.
“They can be counterproductive to recovery and may encourage people to engage in disordered eating behaviours, including restricting or cutting out food groups,” Dr Hungerford explains.
Clinical psychologist Jade Gooding, CEO of the Australia & New Zealand Academy for Eating Disorders agrees that GLP-1s can mask and reinforce underlying eating disorder behaviours.
For example, people may not experience the physical reminder to eat consistently and regularly throughout the day and instead must consciously remind themselves, which can exacerbate a poor relationship with food.
“And all the cognitions around body image and this need to be thin can be further exacerbated because it doesn’t treat the underlying issue,” Ms Gooding says, noting that it doesn’t address core beliefs, self-esteem or body image issues.
However, there’s a lot we don’t know.
With GLP-1s being relatively new, there is not much research involving people with eating disorders. Some evidence suggests they show potential for managing binge eating disorder over three to six months — but the long-term effects are still unknown.
Dr Hungerford says we need more long-term, large-scale studies to see how these medications impact people living with eating disorders—including what happens when they stop using them as weight gain can be triggering for someone experiencing, or at risk of developing, an eating disorder.
Both Ms Gooding and Dr Hungerford say they are increasingly hearing anecdotal reports of people with eating disorders seeking weight loss drugs.
In Healthed’s survey, 48% of GPs reported seeing at least one patient they suspect may have an eating disorder who has asked for a GLP-1 prescription in the last year — including 8% who had encountered 10 or more such patients.
This figure probably underrepresents the issue because binge eating disorder is the most common of all eating disorders, but it can often go unrecognised, including by patients themselves, Ms Gooding says.
“We have this really significant cohort, particularly, but not exclusively of middle-aged women, with binge eating disorder. But we can’t look at someone and determine that they have this diagnosis.”
Alarmingly, 26% of GPs in Healthed’s survey had encountered at least one patient who had obtained a GLP-1 script they thought was not appropriate.
Inappropriate GLP-1 scripts were most likely to have come from commercial telehealth providers, but they weren’t the only source.
While 39% of GPs said these scripts had been obtained via a commercial telehealth provider, 35% said they were from a face-to-face consultation with a GP the patient doesn’t regularly see and 34% said they were obtained from the patient’s usual GP.
Ms Gooding says she is increasingly hearing of people with atypical anorexia or anorexia who have been prescribed GLP-1 medications without consultation with their treatment team.
“Anecdotally, there’s more and more of these presentations coming into eating disorder services,” she says.
“Someone may not look like they are severely underweight or malnourished, but they still meet the criteria for anorexia outside of that,” Ms Gooding says, noting that GLP-1s add to their recovery time and make their presentation trickier.
Even patients with more typical eating disorder presentations may be accessing weight loss medications via telehealth though.
Several GPs in Healthed’s survey said they’d seen patients who’d been prescribed GLP-1s via commercial telehealth despite not meeting the BMI criteria, including one patient with a BMI of less than 18.
Dr Hungerford says telehealth loopholes may be part of the problem.
“We have heard reports of people exaggerating their height and weight when seeking these medications via telehealth, and that makes it difficult for providers to know if the medication is warranted, particularly if there is no face-to-face contact with the patient,” he says.
Ms Gooding says she’s also hearing that basic metabolic screening — such as sit-to-stand, blood pressure and heartrate, for example — isn’t happening over telehealth.
Both Ms Gooding and Dr Hungerford say adequate screening for a history of disordered eating and eating disorders before prescribing GLP-1 RAs is crucial.
Dr Hungerford says weight loss medications must be “critically controlled” in people with a history of disordered eating or eating disorders.
“The risk of fatal consequences for these people is unacceptable,” he says.
He also points out that half of all people with an eating disorder in Australia have larger bodies, and eating disorder rates are increasing most in people of higher weight.
“Despite this, it’s common for people living in larger bodies with eating disorders to experience delayed identification of the eating disorder, misdiagnosis, inappropriate and ineffective treatment, and stigma,” Dr Hungerford says.
Ms Gooding says it’s important to ask about the person’s history of disordered eating thoughts and behaviours, but without a focus on weight, which can intensify body dissatisfaction and feelings of shame.
She suggests questions such as:
For patients who come in proactively seeking weight loss drugs, Ms Gooding recommends asking why they want the medication, what their goal is/the reasons why they want to lose weight and how they think the medication will help them.
It can be an opportunity to pick up new presentations, or help people to understand the extent of their behaviour, she says.
Helpful resources:
The ANZAED Eating Disorder Credential | To become a credentialed eating disorder clinician
The National Eating Disorder Collaboration | Free online eating disorder training for GPs
Management of eating disorders for people with higher weight | Clinical practice guideline
For support with eating disorders and body dissatisfaction, call the Butterfly National Helpline on 1800 ED HOPE (1800 33 4673) or visit www.butterfly.org.au to chat online or email, 7 days a week, 8am-midnight (AEST/AEDT).

Autism Spectrum Disorder – Managing Challenging Behaviours

Paediatric Allergic Rhinitis & Immunotherapy

Premature Ovarian Insufficiency – The New Guidelines

Alcohol Addiction Assessment and Advice


Increase
No change
Decrease
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
