Articles / Should pharmacists get to call themselves ‘doctor’?

The course will be open to registered pharmacists who want to expand their scope of practice, including their prescribing capabilities. Students will complete 48 credit points (8 units) in subjects such as clinical reasoning, interpretation of pathology tests, and quality use of medicines/safe prescribing.
Upon graduation, they can use the DPharm post-nominal and join the ranks of health professionals who call themselves doctors.
While specialist titles are strictly regulated by AHPRA, ‘doctor’ terminology is not afforded quite the same level of protection. People with PhD degrees use it, as do vets, dentists, osteopaths and chiropractors.
In fact, anyone could theoretically call themselves a doctor in Australia, though AHPRA cautions that health professionals must take care when using ‘Doctor’ or ‘Dr’ in their advertising because the public typically equate the term with medical practitioners.
(If a non-medical professional is referred to as Dr in advertising, their specific profession should be clear; e.g. Dr Smith (pharmacist), AHPRA’s guidance states.)
Still, many GPs worry some patients will think pharmacists using the ‘doctor’ title are fully trained medical practitioners.
“Calling oneself ‘doctor’ after a one-year online course risks confusing patients and inflating titles without equivalent responsibility or training,” one respondent wrote.
The AMA agrees the label is confusing, with AMA (WA) President Dr Michael Page saying the association has concerns that patients won’t understand “the enormous difference between a pharmacy graduate who has completed a one-year crash course in diagnostics and therapeutics and a doctor who has completed a decade-long supervised clinical apprenticeship”.
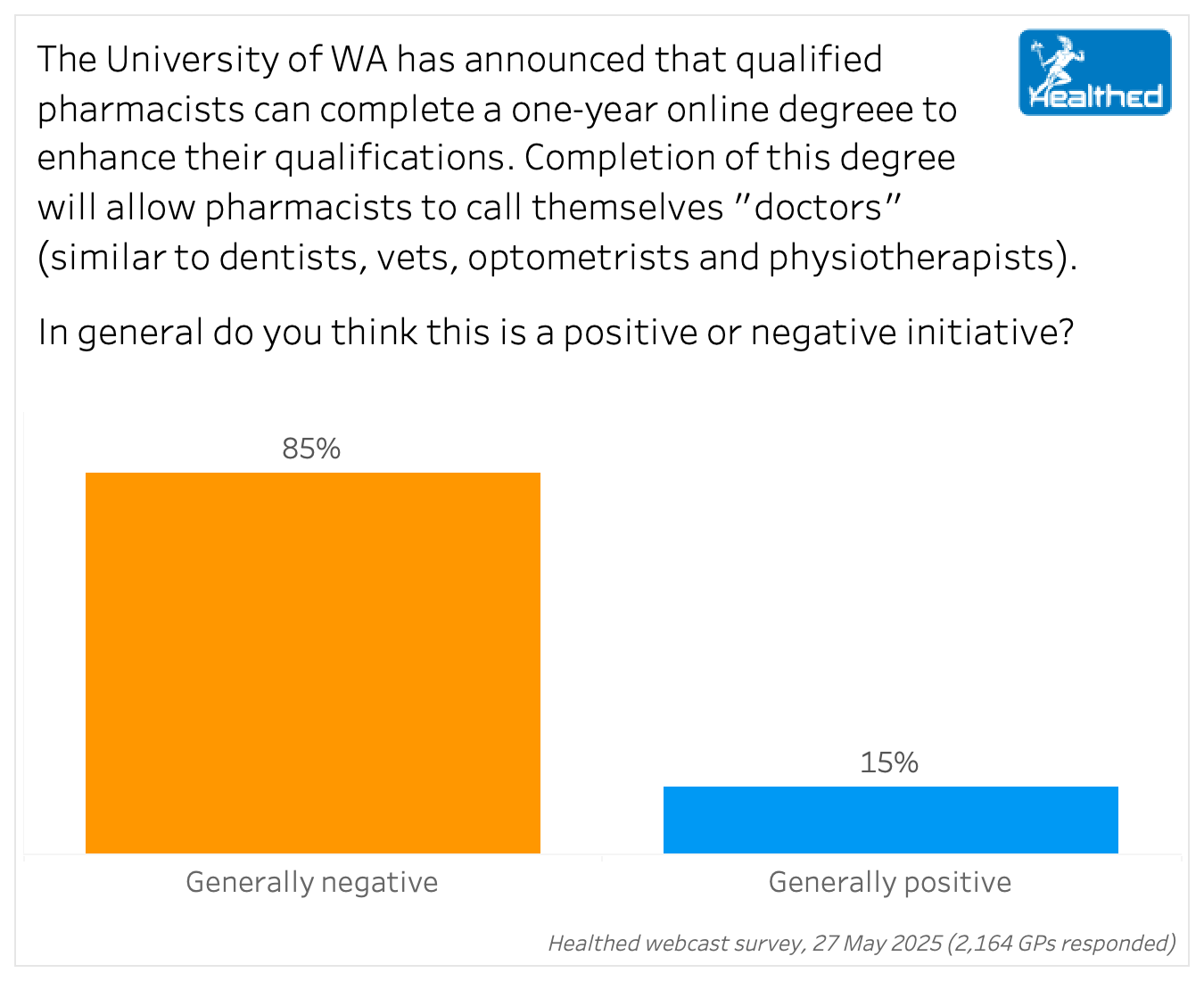
Many GPs in Healthed’s survey commented on the limitations of a year-long online course, with one saying it “does not adequately provide enough clinical exposure and practical experience in dealing with real patients in clinical settings.”
Others opined that the initiative, which comes hot on the heels of Victoria’ s pilot pharmacy prescribing program becoming permanent, devalues medical training and undermines the GP profession. “Why did I study for 10 years if one year is enough?” one GP summed up.
GPs also raised concerns about potential misdiagnosis, inappropriate treatment and poor patient outcomes, as well as fragmentation of care.
“This change risks blurring professional boundaries, undermining team-based care, and creating safety issues if patients assume pharmacists have medical training equivalent to doctors,” one GP commented.
The program could result in “expeditious and superficial assessment, opinion and management that in some instances will lead to inappropriate or incomplete care of the patient,” another wrote.
“Who will be overseeing or monitoring performance/safety/independence of information provided and ensuring it is free from commercial gain?” another GP asked.
There was also unease that pharmacists may be incentivised to prescribe because their income depends on dispensing medication.
Some GPs were worried they’ll end up seeing only the most complex, difficult patients (with little remuneration), or about legal and regulatory issues—like who will be responsible for any adverse patient outcomes.
Fifteen percent of surveyed GPs felt the initiative was positive, citing eased pressure, improved patient access to simple treatments for minor conditions, and benefits for rural and remote communities as upsides.
What your colleagues are saying:
“Everything about it is negative. This initiative makes a mockery of the medical education system and of the personal sacrifice made by all doctors whilst studying for their fellowship/specialisation.”
“While upskilling is valuable, allowing pharmacists to adopt the title ‘doctor’ may confuse patients about their role and clinical scope. Unlike dentists or optometrists who provide diagnosis and treatment within a defined specialty, pharmacists are not trained for comprehensive clinical assessment or management.”
“Creates another group of wanna be doctors who have no idea what is required.”
“Wasn’t it only recently that AMA learnt that the word surgeon shouldn’t be misused, as this misled the public which in turn caused serious harm to the public. Thought society would have learnt to not repeat the same mistake.”
“GPs already struggling, I feel there would be no future for being GP in Australia. On the other hand, patients’ lives would be in danger due to trying to allocate title of doctor to anyone without any experience in medical school.”
“The thin edge of the wedge that will further chop into GP care — mistakes will be made.”
“The whole diagnostic process is a gradually learned skill, explicit formal training and examination and years of observation and practice. A year does not a doctor make.”
“Who takes the responsibility for pharmacy prescriptions? Who manages the side effects on patients’ health?”

Autism Spectrum Disorder – Managing Challenging Behaviours

Paediatric Allergic Rhinitis & Immunotherapy
Premature Ovarian Insufficiency – The New Guidelines

Alcohol Addiction Assessment and Advice


Increase
No change
Decrease
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
