Articles / What’s underlying the gender gap for delayed diagnosis?

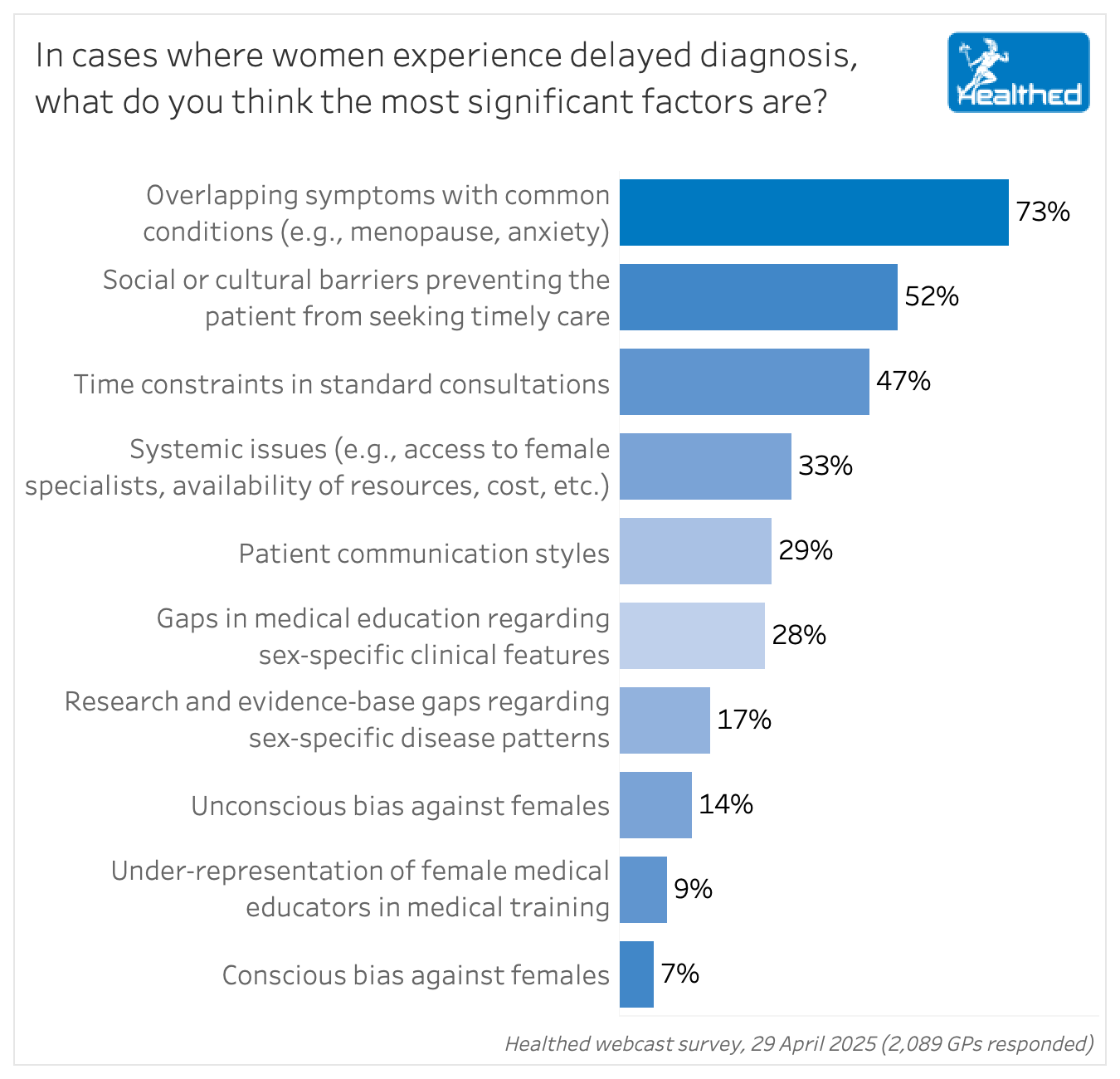
While research shows women do disproportionately experience delayed diagnosis, the reasons are complicated and multifactorial, with nearly three-quarters of GPs (73%) saying the most significant contributing factor is that their symptoms overlap with common conditions.
Social or cultural barriers were the second most common response, cited by 52% of GPs, followed by time constraints, named by 47%.
“Time-limited consultations make it difficult to explore complex or multi-system symptoms, which are often the case in women’s health. More time, better training, and use of decision support tools could help reduce diagnostic delays,” one GP commented.
“It’s important to not write off all issues due to concurrent menopause,” another GP said.
Overall, 54% of GP survey respondents were female and 46% were male. The number of participants who pointed to either unconscious or conscious bias as the cause of delayed diagnosis was small, 14% and 7% of GPs, respectively. But female GPs were twice as likely as their male colleagues to say bias was a significant factor.
“Cultural expectations that it is normal for women to experience symptoms like pain or heavy periods,” can be a major factor, as one GP commented.
“Lack of time and always prioritising others over herself. Females, especially middle aged, are often multitasking – caring for children, parents, husband, running household and working,” another GP noted.
A number of GPs highlighted that there may be particular challenges for women from migrant or culturally and linguistically diverse backgrounds.
One third of GPs said systemic issues were among the most important factors.
“Lack of Medicare funding for complex consults, and gender pay gap in general practice leading to lack of practitioner availability,” one GP commented.
“Government has insisted on sooo much red tape that consult time is even more pressured,” another GP said.
What your colleagues are saying
“Many doctors have been, and still are, very anti menopausal hormone therapy and may therefore have had bias against MHT, not necessarily females; hence women have ’put up’ with symptoms for some time.”
“More research is required into the differences in symptoms that women present with compared to men, in the 21st century it is about time that women and other racial groups apart from Caucasians were represented equally in clinical trials.”
“Often men are the ones who don’t go to the GP at all, and are more likely to get delayed diagnoses for lots of things.”
“Patients ignoring their symptoms and putting their families and work first.”
“Silent and late symptoms resulting in delay of diagnosis.”
“Not attending screening tests in a timely manner.”
“Lack of available GPs and patients may just give up attempting to get an appointment.”
“Long waits for GP appointments and lack of continuity of care… I suspect males also experience delayed diagnoses too. Sometimes the patient is very complex with multiple confusing comorbidities.”
“Misogyny is too emotionally charged a word to use as is seen in the media. It is a failure of communication between doctor and patient – probably due to a lack of time in the consultation.”
“Cost is the most significant factor. My patient who can’t afford private health insurance is still waiting for a diagnostic and therapeutic laparoscopy for suspected endometriosis two years since her gynae appt at public hospital.”
“Fear of a diagnosis based on observed experiences of other women.”
“By offering double appointments to women for complex conditions, which I always do, I am putting myself at a financial disadvantage, hence widening the already existing gender pay gap in GP.”
“Men get misdiagnosed as well. I think the public does not realise how many errors can be made, or the wide variety of overlapping conditions. They expect that their rare condition will be diagnosed on the first appointment – not realistic especially with 15-minute appointments for GPs. ED departments are also not funded to explore difficult diagnoses. Patients take misdiagnosis personally, not realising the difficulty in making a diagnosis.”

Postural Orthostatic Tachycardia Syndrome in Women

Panel Discussion on The Role of GLP-1 in the Management of CKD in T2D

Big Heads & Small Heads

Peanut Allergy


It should only change if there's clear evidence that a new model is better
it should remain independent and locally governed
it should be replaced with an untested national model
Listen to expert interviews.
Click to open in a new tab
Browse the latest articles from Healthed.
Once you confirm you’ve read this article you can complete a Patient Case Review to earn 0.5 hours CPD in the Reviewing Performance (RP) category.
Select ‘Confirm & learn‘ when you have read this article in its entirety and you will be taken to begin your Patient Case Review.
