What Causes Fibromyalgia?
Fibromyalgia is something of a mystery. It can’t be detected with scans or blood tests, yet it causes lifelong pain for millions of people.
The disease mainly affects women (about 75-90% of cases), causing pain all over the body. Because not all healthcare professionals are adept at identifying and diagnosing fibromyalgia, reported rates of the condition vary greatly from country to country. In China, it affects only 0.8% of people, in France around 1.5%, in Canada 3.3%, and in Turkey 8.8%. Estimates in the US range from 2.2% to 6.4%, and in Russia, about 2% of the population is affected.
People with the condition are often diagnosed if they have longstanding muscle pain, bone or joint pain and fatigue. Fibromyalgia can also cause insomnia, “brain fog”, some symptoms of depression or anxiety, as well as a range of other complaints, including irritable bowel syndrome and headache. Many patients are also hypermobile (“double-jointed”), and there is some overlap with chronic fatigue syndrome (also known as ME).
Guidelines from the American College of Rheumatology make it clear that the diagnosis should be made using defined criteria based on the “widespread pain index” (which scores the number of painful regions out of 19) coupled with a symptom severity scale. The diagnosis also takes fatigue, generalised pain, unrefreshing sleep and cognitive symptoms into account. It doesn’t matter if the patient has another rheumatic disease, they can still be diagnosed with fibromyalgia.
The scoring system, recommended by the American College of Rheumatology, is often used in clinical trials, but in the clinic, most doctors rely on detecting tender points in specific places and on excluding other medical conditions, including rheumatic conditions. Unlike say, rheumatoid arthritis or lupus, the tests do not show clear evidence of inflammation or autoimmunity (when the body’s immune system attacks itself) and scans are normal.
The lack of inflammation or structural abnormality in muscles or joints – aside from making diagnosis difficult – is the main reason there are no widely accepted or effective treatments. In rheumatic diseases, where we understand the mechanisms that underlie the condition, we have the most effective treatments. In rheumatoid arthritis, for example, we know that much of the inflammation is caused by a cell-signalling protein (cytokine) called tumour necrosis factor and that blocking the activity of this protein switches off the disease in most patients.
A number of possible mechanisms have been proposed in fibromyalgia, including abnormal muscle metabolism, reduced levels of steroid hormones such as cortisol, or abnormal small nerve fibres. But these abnormalities aren’t found in all patients with the condition. As such, they can’t be used as part of a diagnostic test, nor can they help develop treatments.
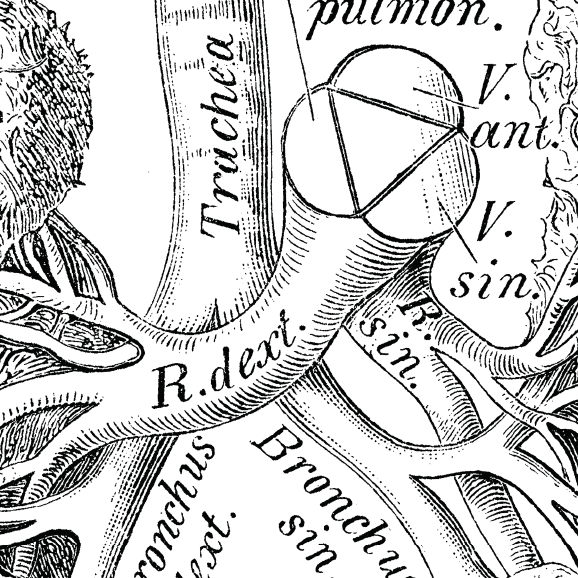
Some experts have suggested that fibromyalgia may be related to abnormalities in the autonomic nervous system – the part of the nervous system that controls bodily functions, such as heart rate and blood pressure – and how the brain responds to pain signals and reacts to external stressors (such as infections). But there is currently no hard evidence to back up this theory.
Looking for clues
To fill in some of the gaps in our knowledge about this devastating condition, our research team at Brighton and Sussex Medical School is investigating the potential role of the autonomic nervous system and inflammation in fibromyalgia and chronic fatigue syndrome.
For our study, we have two groups of patients: one with pain as the main symptom and the other with fatigue as the main symptom. We also have matched controls – people without the disease, but otherwise similar characteristics – to make meaningful comparisons.
The study is in two parts. First, we will test the patients’ autonomic nervous system using a tilt-table. This involves tilting the person head downwards to see how well their body adapts to this change in posture by changing heart rate and blood pressure (both of which are monitored during the test).Second, we will stimulate patients’ immune systems with a typhoid vaccine (the normal type used in travellers) and perform magnetic resonance brain scans to look for changes in blood flow and also measure the levels of “inflammatory mediators” (the chemicals the body produces in response to stimuli of this type), to see whether these are higher in the fibromyalgia patients.
Our study should, for the first time, help us to address the question of whether there really is an abnormal brain response to inflammation or infection in these patient groups and enable us to explore the relationship between the abnormal functioning of the autonomic nervous system and fibromyalgia and chronic fatigue syndrome.
Fibromyalgia rarely goes away and treatment options are limited. Only by developing a proper understanding of the disease processes underlying this condition will doctors be able to make a clear, positive diagnosis, and most importantly, offer effective therapy.
Disclosure Statement
Kevin Davies receives funding from AR-UK.
Jessica Eccles receives funding from Academy of Medical Sciences, National Institute of Health Research, MQ
Neil Harrison receives funding from the Wellcome Trust, Medical Research Council (MRC), Arthritis Research UK, and Janssen Pharmaceuticals.
Type 2 Diabetes: Individualising Care, Beyond Metformin
The object of this article is to assist the readers to make simpler Type 2 Diabetes management choices for themselves and patients.
Fetal Fraction – The Essential Factor in Non-Invasive Prenatal Testing

Non-Invasive Prenatal Testing (NIPT), the cell-free DNA-based blood test that screens for fetal chromosomal abnormalities, is fast becoming a routine part of obstetric care.
NIPT at a glance
During pregnancy, maternal plasma contains fragments of DNA from the mother and from the placenta (fetal DNA).
The proportion of DNA fragments from particular chromosomes is usually very stable throughout pregnancy. If there is an excess of fetal fragments from one chromosome, the proportion of fragments from that chromosome will be changed.
Inconclusive tests
A key reason that NIPTs should precisely measures the amount of fetal DNA in the sample – the fetal fraction – is if there is insufficient fetal DNA, the result may merely reflect the genetic status of the mother.
NIPT assays should report a result only if there is sufficient fetal DNA to be confident of accuracy.
Rarely, a test for trisomy 21,18 and 13 cannot be reported.
This occurs in 3% of women tested by Sonic Genetics and is usually because there is insufficient fetal DNA compared with maternal DNA in the mother’s plasma.
This low fetal fraction can be due to a relative excess of maternal DNA and this can vary over time. It is more common in women with increased body weight, and more likely in the presence of infection and inflammation, or after exercise.
It also occurs if the mother or fetus has some subtle benign variations in chromosome structure (copy number variants) that make estimating the proportion of fragments from a chromosome unreliable.
In some instances, the DNA in the sample has degraded during collection and shipping to the laboratory, and the quality is insufficient for a reliable result. These factors interfere with quality control of the test.
Two thirds of women will get a result on re-testing.
However, if the second test is inconclusive, it should not be repeated. This occurs in 1% of pregnant women screened.
It is also not worth using another form of non-invasive prenatal test. Other tests do not estimate the fetal fraction accurately and may provide false reassurance.
A decision about other test modalities (combined first trimester screen, second trimester serum screen, detailed ultrasonography or invasive genetic testing such as CVS/amniocentesis) should be based on assessment of all identified risk factors and may require specialist consultation.
More rarely (in 0.5 –1% of women) the test reports a result for trisomy 21, 18 and 13 but not for fetal gender and sex chromosome abnormalities. It is unlikely that a repeat test will provide a result. A decision about using fetal ultrasound or invasive genetic testing to document fetal gender should be based on assessment of need and any identified risk factors.
General Practice Pathology is a new regular column each authored by an Australian expert pathologist on a topic of particular relevance and interest to practising GPs.
The authors provide this editorial, free of charge as part of an educational initiative developed and coordinated by Sonic Pathology.
New Medicare-Funded BRCA Testing – Use With Caution

GPs may have to correct some patients’ misunderstanding following reports in the general media suggesting that testing for high risk cancer genes was now available to everyone free of charge.
Writing in the latest issue of the MJA, Australian genetics experts say that testing for specific high- risk genetic mutations, especially BRCA1 and BRCA2 has been available to appropriate patients free of charge (but not Medicare-rebated) by genetic specialists in public clinics for over 20 years.
What’s new is that these tests now attract a Medicare rebate and you don’t have to be a genetic specialist to order them, but they are still only available to selected patients.
“Testing is appropriate when there is at least a 10% chance of identifying a gene mutation responsible for the personal or family history of cancer,” the authors of the article wrote.
There are a number of algorithms available to help clinicians calculate whether the likelihood of having one of these cancer-causing genetic mutations is at least 10%.
Usually testing is initially considered for patients who have been diagnosed with either breast or ovarian cancer, and because of their young age and/or their strong family history are considered at high possibility of having a genetic mutation that explains their condition.
The new item numbers (73295,73296 and 73297) cover testing for heritable germline mutations in seven genes including BRCA1 and BRCA2. If such a mutation is found, then at risk adult relatives will be justified in also accessing testing.
However, as the article authors point out there are limitations with this type of genetic testing. Firstly most breast and ovarian cancers occur in people without an identifiable underlying genetic variant.
“Only 5% of female breast cancers, 15% of invasive epithelial ovarian cancers and up to 14% of male breast cancers are related to BRCA1 or BRCA2 mutations, thus, most patients with breast cancer do not need, nor will they benefit from, a genetic test,” they said.
That’s not to say the absence of BRCA1 or BRCA2, or one of the other rarer high-risk mutations currently tested for, excludes the possibility that the patient has inherited a predisposition to the cancer. Families that appear to have a high prevalence of these types of cancer may indeed have an inherited genetic mutation, it is just that because of limitations of technology and knowledge it is yet to be isolated.
What’s more, the sensitivity of the current testing methods, means that a number of incidental genetic mutations may be noted, but the significance of these is as yet unknown. It is critical that when testing is requested for a relative of an affected patient, the laboratory is informed of the exact genetic variation found in the original affected patient, to ensure pathologists distinguish between the disease-causing mutation and variants of undetermined significance. The authors also suggest confining testing to only the most likely variant/s rather than requesting testing for mutations in multiple genes.
“[T]he testing of multiple genes may uncover unclassified variants, variants outside the usual clinical context, variants unrelated to the current cancer, or unexpected important variants for which the patient has not been well prepared,” they said.
They also suggest education and counselling be given to patients considering this genetic testing, and written consent obtained.
The new Medicare item numbers represent a major step forward in terms of genetic and genomic testing becoming mainstream, but, as the current incorrect media headlines demonstrate, this transition is going to require information and education. Clinicians who order these tests are likely to benefit from establishing close ties with genetic services and specialists to ensure best and appropriate practice in this ever-expanding area of medicine.
Ref:
Med J Aust 2018; 209 (5): 193-196. || doi: 10.5694/mja17.01124
Detecting and treating Mycoplasma genitalium

Mycoplasma genitalium (M. genitalium), is thought to affect up to 400,000 Australians.
It causes urethritis in men, and in women it can lead to pelvic inflammatory disease, cervicitis and preterm labour. It is also a recognised cause of anorectal proctitis along with other infections including Chlamydia trachomatis (including the LGV strains), gonorrhoea, syphilis, HSV and shigellosis.
Asymptomatic infection is also common.
Who to test
Only test those with symptoms and their contacts. Screening asymptomatic people for M. genitalium is not currently recommended.
Diagnosis
Females:
PCR on endocervical or vaginal swab, first pass urine (FPU), ThinPrep -collected by cervical brush/swab.
Males:
PCR on urethral swab (in preference to FPU), anorectal swabs.
Throat swabs are not recommended as pharyngeal infection is uncommon.
Transport: Ambient temperature; if there is any delay from collection to transport to the laboratory, the sample must be refrigerated
Current treatment recommendations
Preliminary data from the patient populations suggests resistance rates to macrolides may be as high as 64 per cent.
The highest rates are likely to be in the men who have sex with men (MSM) population. Although information regarding fluoroquinolone resistance (moxifloxacin) is not available with this test, some studies suggest resistance to fluoroquinolones is present in 10–15% of infections.
Doxycycline alone is ineffective in two-thirds of infections but will lower bacterial load in most cases, increasing the likelihood of cure with a subsequent antibiotic.
Pretreating M. genitalium infections with doxycycline for one week and then treating susceptible infections with azithromycin and macrolide-resistant infections with a fluoroquinolone eradicates >90% of infections.
Current treatment regimens
Macrolide sensitive
Doxycycline 100mg bd for seven days followed by azithromycin 1g stat then 500mg daily for three days (total 2.5g)
OR
Doxycycline 100mg bd for seven days followed by azithromycin 1g single dose.
It is not known to what extent the improved outcomes resulting from the use of doxycycline followed by 2.5g azithromycin are due to this dose of azithromycin, rather than simply the pre-treatment with doxycycline.
The higher dose of azithromycin requires a private prescription.
Macrolide resistant
Doxycycline 100mg bd for seven days followed by moxifloxacin 400mg daily for seven days. A longer course of moxifloxacin may be required in women with pelvic inflammatory disease.
Moxifloxacin requires a private prescription, cannot be used in pregnancy and is expensive. It is associated with diarrhoea, occasional tendinopathy and rare neurological and cardiac events.
Treatment failures following appropriate fluoroquinolone treatment may require specialist advice.
Additional actions
Advise no sex without condoms until tested for cure (14 days after completion of treatment).
Advise no sex with untested previous sexual partners.
Test of cure
Test of cure by PCR should be done at least two weeks after treatment is completed i.e. four weeks after commencing therapy.
Contact tracing
In heterosexuals, the risk of PID and reproductive complications suggests a greater need to trace, test and treat infected contacts.
The time period for contact tracing is unknown.
Asymptomatic infection and macrolide resistance are more common in MSM and there is only limited evidence that this is harmful. As moxifloxacin will probably be required for treatment, contact tracing may be best confined to continuing partners of a symptomatic person.
References:
Australian STI Management Guidelines for Use in Primary Care
http://www.sti.guidelines.org.au/sexually-transmissible-infections/mycoplasma-genitalium#management
Australian Contact Tracing Manual contacttracing.ashm.org.au/conditions/when-contact-tracing-is-recommended/mycoplasma-genitalium
General Practice Pathology is a new regular column each authored by an Australian expert pathologist on a topic of particular relevance and interest to practising GPs.
The authors provide this editorial, free of charge as part of an educational initiative developed and coordinated by Sonic Pathology.
Hyperhidrosis: Not Just A Cosmetic Problem

This article provides an overview of the clinical approach, investigation and management of hyperhidrosis.
COPD Updates: Pharmaceutical Benefits Advisory Committee Recommendations about Inhaled Medications
This article discusses the updated recommendations for use of inhaled medications in patients with chronic obstructive pulmonary disease, effective 1 August 2018.
Treating depression in MI patients saves lives

Effectively treating depression in patients who have just experienced a heart attack will not only improve their quality of life, it could well improve their mortality, new research from Korea suggests.
Among 300 patients who had recently experienced acute coronary syndrome and had depression as a comorbidity, those randomised to a 24-week course of escitalopram were 30% less likely to have a major adverse cardiac event over a median of eight years compared with those given placebo.
In actual numbers, 40.9% (61)of the 149 patients given escitalopram had a major adverse event (including cardiac death, MI or PCI) over the period of follow-up compared with 53.6% (81) of the placebo group (151 patients), according to the study findings published in JAMA.
It has long been known that depression is a common morbidity associated with acute coronary syndrome. It is also known that patients who have this comorbidity tend to have worse long-term cardiac outcomes than those who are depression-free.
But what has yet to be proven is the benefit of treating this depression, at least in terms of mitigating this increased risk of a poor cardiac outcome. To date studies on the topic have yet to prove a significant benefit, with research providing conflicting results.
According to the study authors, in this trial there was a significant correlation between improvement in the depression and better protection against major cardiac events. Even when they excluded those people who were still taking the antidepressant one year after the acute coronary syndrome, the protective effect was still present. Consequently, they hypothesised that the protection was more a reflection of the successfully treatment of the depression rather than the particular medication.
This was consistent with a trend seen in previous research using different medications and treatments. However, the better result could be because escitalopram is more effective in treating acute coronary syndrome depression than other agents that were studied previously, the authors suggested.
“Escitalopram may have modifying effects on disease prognosis in ACS-associated depressive disorder through reduction of depressive symptoms,” the study authors suggested.
There were a number of caveats with regard this study that the authors said needed to be considered. These included the fact the cohort was entirely Korean which may have caused an ethnic bias, the depressive symptoms were less severe than in previous studies (though this was more likely to lead to the effect being an under-estimate) and also the severity of the underlying heart disease (namely heart failure) was relatively low.
Nonetheless the researchers were able to conclude that among patients with depression who had had a recent acute coronary event, 24 weeks of treatment of escitalopram significantly reduced the risk of dying or having a further adverse cardiac event after a median of 8.1 years.
How generalisable these findings are, will need to be the subject of further research.
Ref:
JAMA 2018;320 (4): 350-357. Doi: 10.1001/jama.2018.9422
Study: Vitamin D unlikely to protect individuals from brain-related disorders.

New research from South Australian scientists has shown that vitamin D (also commonly known as the sunshine vitamin) is unlikely to protect individuals from multiple sclerosis, Parkinson’s disease, Alzheimer’s disease or other brain-related disorders.
The findings, released today in the science journal ‘Nutritional Neuroscience’ reported that researchers had failed to find solid clinical evidence for vitamin D as a protective neurological agent.
“Our work counters an emerging belief held in some quarters suggesting that higher levels of vitamin D can impact positively on brain health,” says lead author Krystal Iacopetta, PhD candidate at the University of Adelaide.
Based on a systematic review of over 70 pre-clinical and clinical studies, Ms Iacopetta investigated the role of vitamin D across a wide range of neurodegenerative diseases.
“Past studies had found that patients with a neurodegenerative disease tended to have lower levels of vitamin D compared to healthy members of the population,” she says.
“This led to the hypothesis that increasing vitamin D levels, either through more UV and sun exposure or by taking vitamin D supplements, could potentially have a positive impact. A widely held community belief is that these supplements could reduce the risk of developing brain-related disorders or limit their progression.”
“The results of our in-depth review and an analysis of all the scientific literature however, indicates that this is not the case and that there is no convincing evidence supporting vitamin D as a protective agent for the brain,” she says.
Source: News Medical Net
Using HbA1c Wisely

Glycated haemoglobin (HbA1c) has been used for monitoring patients with established diabetes for many years but its diagnostic application is a more recent development. This article provides some background to the test, explains dual reporting of results and discusses the use of HbA1c in the diagnosis and monitoring of diabetes.
What is HbA1c?
Adult haemoglobin is predominantly (97% of total) HbA. HbA1c is formed when a glucose molecule non-enzymatically attaches to the N-terminal valine of the β-chain of HbA.
The amount of HbA1c formed is directly proportional to the average plasma glucose concentration during the 120-day life span of the erythrocyte, with recent plasma glucose contributing more than earlier concentrations. HbA1c is therefore a reflection of the average glycaemia over roughly the preceding 6–8 weeks and has a vital role in assessing the risk of an individual developing the complications of diabetes.1
HbA1c for the diagnosis of diabetes mellitus
A 2012 position statement of the Australian Diabetes Society, the Royal College of Pathologists of Australasia (RCPA) and the Australasian Association of Clinical Biochemists (AACB)2 contains the following:
- HbA1c levels ≥6.5% (≥48 mmol/mol) are acceptable for diagnosing diabetes so long as the test is done in a laboratory and no conditions exist which preclude its accuracy.
- In an asymptomatic patient with a positive result, the test should be repeated to confirm the diagnosis.
- The existing criteria based on fasting and random glucose levels and on the oral glucose tolerance test remain valid and are the diagnostic tests of choice for gestational diabetes, type 1 diabetes and in the presence of conditions that interfere with HbA1c measurement.
The use of HbA1c simplifies the diagnostic process and may facilitate the detection of diabetes diagnosis. The test can be performed at any time of the day, does not require special pre-test preparation, such as a diet or fasting, and is stable when collected in the appropriate specimen tube.
Testing should be restricted to patients at high risk of undiagnosed diabetes and who are asymptomatic.3 If one or more symptoms suggestive of diabetes are present in a low-risk patient, blood glucose tests should be used, because patients with rapidly evolving diabetes can have normal HbA1c.
HbA1c <6.5% (<48mmol/mol) indicates that diabetes is unlikely but (since the patient is high-risk) the test should be repeated in 12 months. Patients should be given appropriate lifestyle advice and other modifiable cardiovascular risk factors should be assessed.3
There is uncertainty about the use of HbA1c to diagnose prediabetes. While patients with HbA1c above normal but below 6.5% (48 mmol/mol) are more likely to develop diabetes than is suggested by their AUSDRISK score alone, they have minimal risk of developing microvascular complications. Management is the same as for those at high risk of type 2 diabetes with HbA1c within the normal range.3
HbA1c ≥6.5% (≥48 mmol/mol) should be confirmed by another test (glucose or repeat HbA1c). Repeat HbA1c should be performed on a different day but as soon as possible, before any lifestyle or pharmacological interventions are initiated.3 It is important that clinicians state clearly the indication for the test when requesting HbA1c testing, with wording such as ‘diabetes monitoring’ or ‘diabetes screening’. This will allow the correct Medicare item number and interpretative comments to be used.
Individualisation of HbA1c treatment targets
In monitoring patients with established diabetes, the general target is ≤7.0% (≤53 mmol/mol). Individualisation of target HbA1c, taking into account patient-specific factors, such as type of diabetes and its duration, pregnancy, diabetes medication used, existing cardiovascular disease, risk of hypoglycaemia and comorbidities, may modify the target range from ≤6.0% (≤42 mmol/mol) to ≤8.0%(≤64 mmol/mol).4
Dual reporting of HbA1c
There are many assays for measuring HbA1c. For many years, the NGSP in the US and other national and regional programs harmonised HbA1c methods. This allowed valid, interlaboratory comparison of results. The NGSP uses percentage (%) units. The IFCC standardised glycated haemoglobin measurement by making it traceable to an international standard.5 The IFCC uses mmol/mol (mmol HbA1c per mol total Hb).
The improved specificity of IFCC-HbA1c is reflected in results which are consistently 1.5%–2.0% lower than NGSP values.1
A 2007 consensus statement from the American Diabetes Association (ADA), European Association for the Study of Diabetes (EASD), IFCC and International Diabetes Federation (IDF) was adopted and implemented by Australasian laboratories.5
It recommended that HbA1c results be reported in both IFCC units (mmol/mol) and derived NGSP units (%) to allow clinicians to become familiar with IFCC results before reporting of NGSP % units is withdrawn. Currently, there is no agreement on when dual reporting will cease and hence HbA1c results are still reported with two units.
Conditions affecting HbA1c results
As HbA1c is simply haemoglobin with the addition of a glucose molecule, conditions that affect red blood cells or their survival time, such as haemoglobinopathies or anaemia, will affect the HbA1c result.3
Patients with abnormal haemoglobins may form other glycated products which may form at different rates to that of normal haemoglobin.
Haemolytic anaemia can reduce HbA1c by decreasing red cell survival, leading to reduction in the availability of haemoglobin for glycation. This occurs with autoimmune haemolytic anaemia, haemoglobinopathies and chronic renal failure.
Any drugs that give rise to haemolytic anaemia will have the same effect. Red cell survival time is also reduced in severe liver disease, anaemia of chronic disease, vitamin B12 and folic acid deficiencies, and regular phlebotomy. Interestingly, iron deficiency anaemia can increase HbA1c by up to 2%.1 There are alternative ways of monitoring diabetes treatment in these patients, including the use of closer glucose monitoring and fructosamine testing.
Any discordance between glucose and HbA1c levels should alert the clinician so that other testing options should be considered.
Key points
When requesting HbA1c it is vital that the clinician specify clearly the indication for the test, for example, ‘diabetes monitoring’ or ‘diabetes screening’.
- HbA1c ≥6.5% (≥48 mmol/mol) can be used to diagnose diabetes in asymptomatic, high-risk patients. HbA1c ≥6.5% should be confirmed with glucose or another HbA1c performed on a different day but as soon as possible, before any intervention has commenced.
- The recommended treatment target is HbA1c ≤7.0% (≤53 mmol/mol). Treatment targets may need to be individualised to between ≤6.0% (≤42 mmol/mol) to ≤8.0% (≤64 mmol/ mol), depending on patient-specific factors, such as type and duration of diabetes and risk of hypoglycaemia.
- Currently, HbA1c is reported in both National Glycohemoglobin Standardization Program (NGSP) units (%) and International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) units (mmol/mol), with the aim of eventually reporting in IFCC units only.
- A number of medical conditions affect HbA1c results and preclude its use in both monitoring and diagnosis of diabetes mellitus.
References
- Kilpatrick ES. Haemoglobin A1c in the diagnosis and monitoring of diabetes mellitus. J Clin Pathol 2008;61(9):977-982
- d’Emdem MC. et al. The role of HbA1c in the diagnosis of diabetes mellitus in Australia. MJA 2012;197(4):1-3
- d’Emdem MC. et al. Guidance concerning the use of glycated haemoglobin (HbA1c) for the diagnosis of diabetes mellitus – A position statement of the Australian Diabetes Society. MJA 2015;203(2):89-91
- Cheung NW. et al. Position statement of the Australian Diabetes Society: individualisation of glycated haemoglobin targets for adults with diabetes mellitus. MJA 2009;191(6):339-344
- Jones G. et al. Consensus Statement on the Worldwide Standardisation of the Haemoglobin A1c Measurement – An Australasian Update. The Clinical Biochemist Newsletter 2008;14-18. Available online: https://www.aacb.asn.au/documents/item/1213
General Practice Pathology is a new regular column each authored by an Australian expert pathologist on a topic of particular relevance and interest to practising GPs.
The authors provide this editorial, free of charge as part of an educational initiative developed and coordinated by Sonic Pathology.
Evidence-based Refinement of the Diagnosis and Management in Chronic Obstructive Pulmonary Disease
This article discusses the recent refinements to the diagnosis and management of chronic obstructive pulmonary disease.
Mammographic Breast Density: A New Era for Breast Cancer Screening and Prevention
This article discusses how high mammographic breast density lowers the sensitivity of breast cancer screening and increases breast cancer risk.